Patient Billing Automation
Introduction
The Patient Billing Automation feature is designed to simplify and optimize your Patient Billing workflow by automatically sending Invoices and payment reminders to Patients once their insurance claims have been processed. If your Practice has Secondary Claim Processing enabled, the system will automatically wait until the secondary claims are fully processed before including those Invoices in the automation.
Instead of manually tracking claim completion, preparing statements, and following up for payments, the system intelligently handles these steps for you.
This automation reduces the manual effort required by billers, minimizes delays in sending statements, and ensures timely and consistent communication. It also helps improve Patient collection while reducing the billing workload.
Key Functionalities
- Automatically sends initial Invoice notification to Patients with a secure payment link.
- Sends reminder emails or text messages based on your configured schedule.
- Let you define your billing cycle frequency—on a specific weekday, monthly, or twice a month.
- Allows configuration of reminder frequency.
- Option to continue sending reminders until the Invoice is fully paid.
- Ability to exclude Invoices based on specific criteria such as Patient credits, card on file, recurring profile, small balances, etc.
- Choose preferred communication modes—Email, Text, or PHR.
- Option to send multiple outstanding Invoices of a Patient as a single consolidated statement.
- Provision to track automation progress—including Invoices scheduled, sent, and excluded—from a dedicated dashboard.
- Enabling Patient Billing Automation
- Configuring Billing Cycle Frequency
- Enabling Automation for 'Initial Communication' and 'Reminders'
- Excluding Invoices from Automatic Patient Billing
- Wait Period Before Including Invoice in Automation
- Configuring Initial Communication Settings
- Configuring Automation for Reminders
- Configuring Reminder Settings
- Handling Invoices Not Paid After Three Reminders
- Tracking the Patient Billing Automation Progress
Note: If RCM is enabled for your Practice, the Patient Billing Automation feature can be configured only in either RCM or CharmHealth EHR.
Enabling Patient Billing Automation
To enable sending Invoices automatically to Patients, navigate to 'Settings > Billing > Patient Billing' and choose 'Yes' for 'Enable Patient Billing Automation'.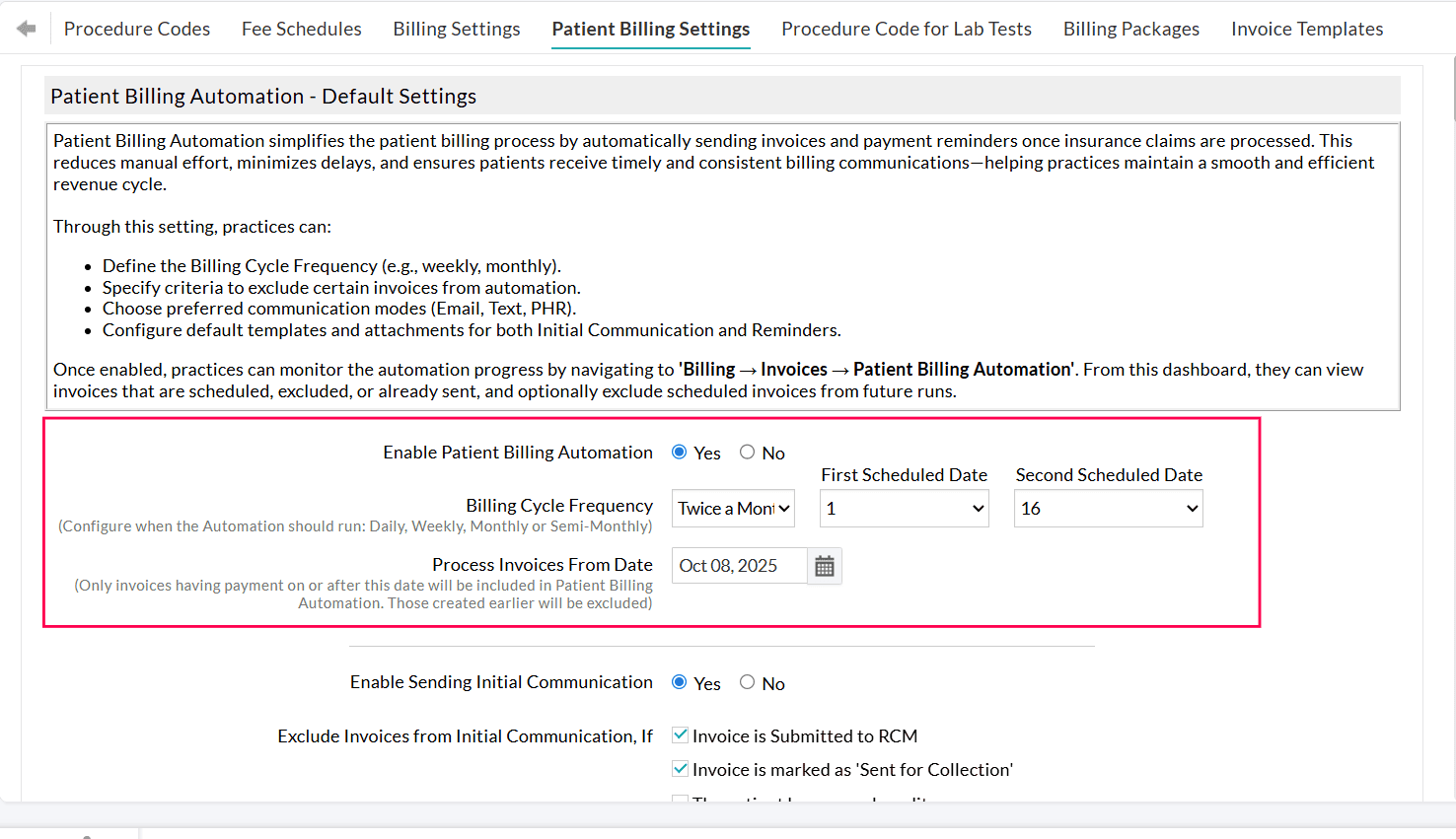
Once enabled, Practices can track the automation status from 'Billing > Invoices > Patient Billing Automation'. This dashboard displays Invoices that are scheduled, excluded, or already sent, and allows Practices to manually exclude specific scheduled Invoices from future runs.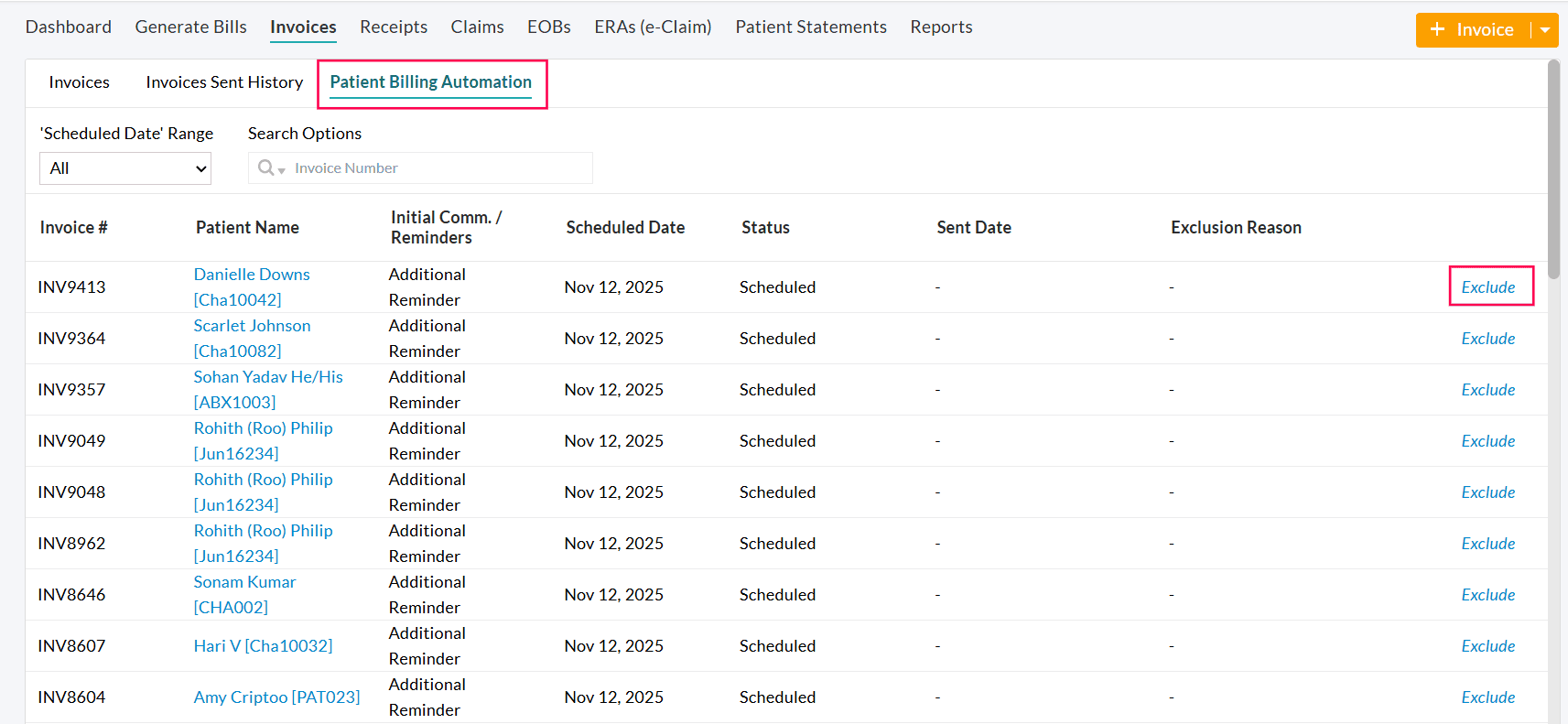
Which Invoices are Included in Patient Billing Automation?
- Invoices for which the Claims are processed and have a PR balance Due are included in the Patient Billing Automation.
- Invoices for which the Secondary Claims are fully processed are included in the automation.
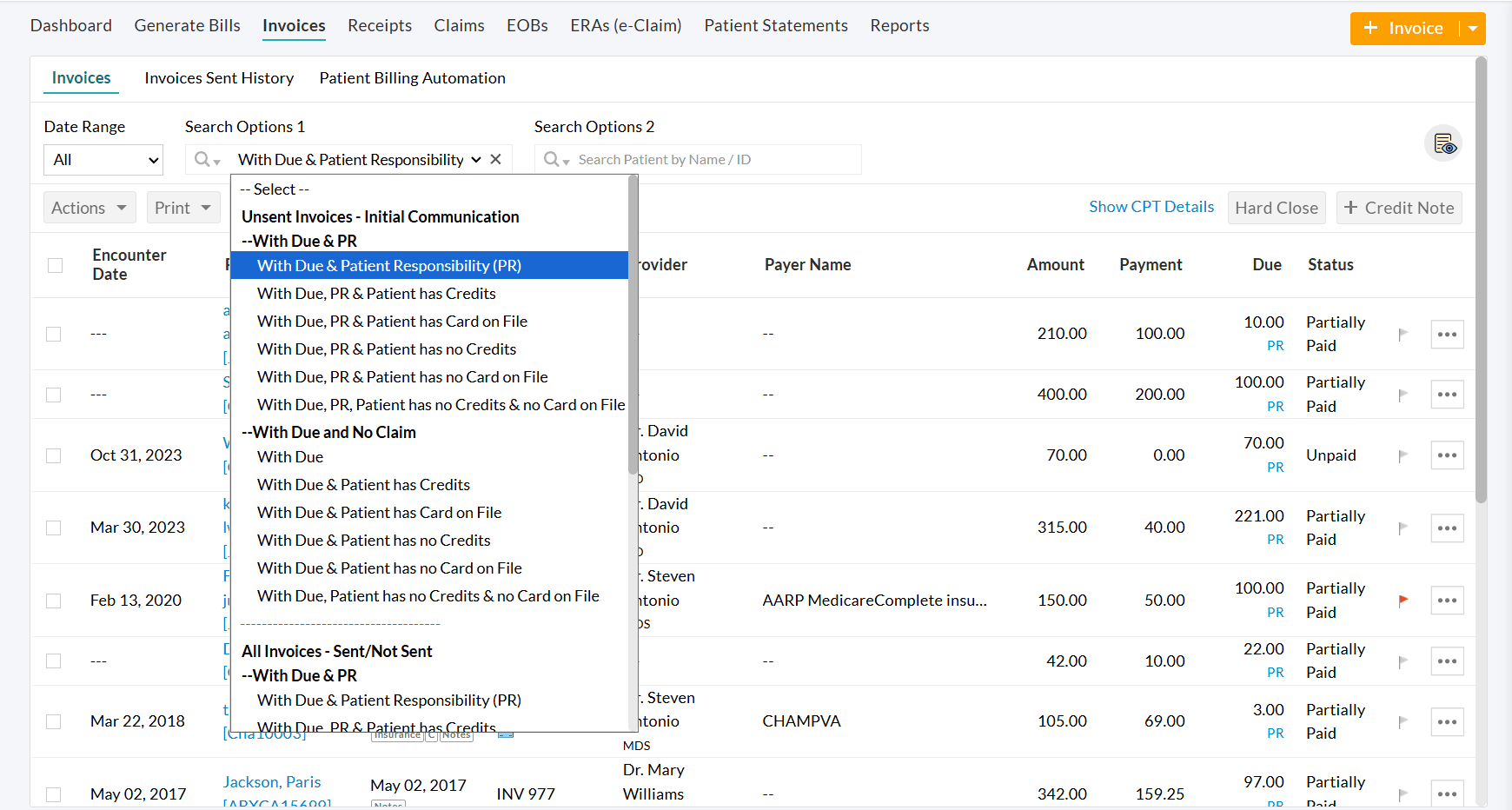
- All Invoices under the filter 'Billing > Invoices > Search Options 1 > Patient Billing - Initial communication > With Due and Patient Responsibility' are automatically considered for initial communication automation.
- All Invoices, except those that fall under any configured exclusion criteria, are processed through automation.
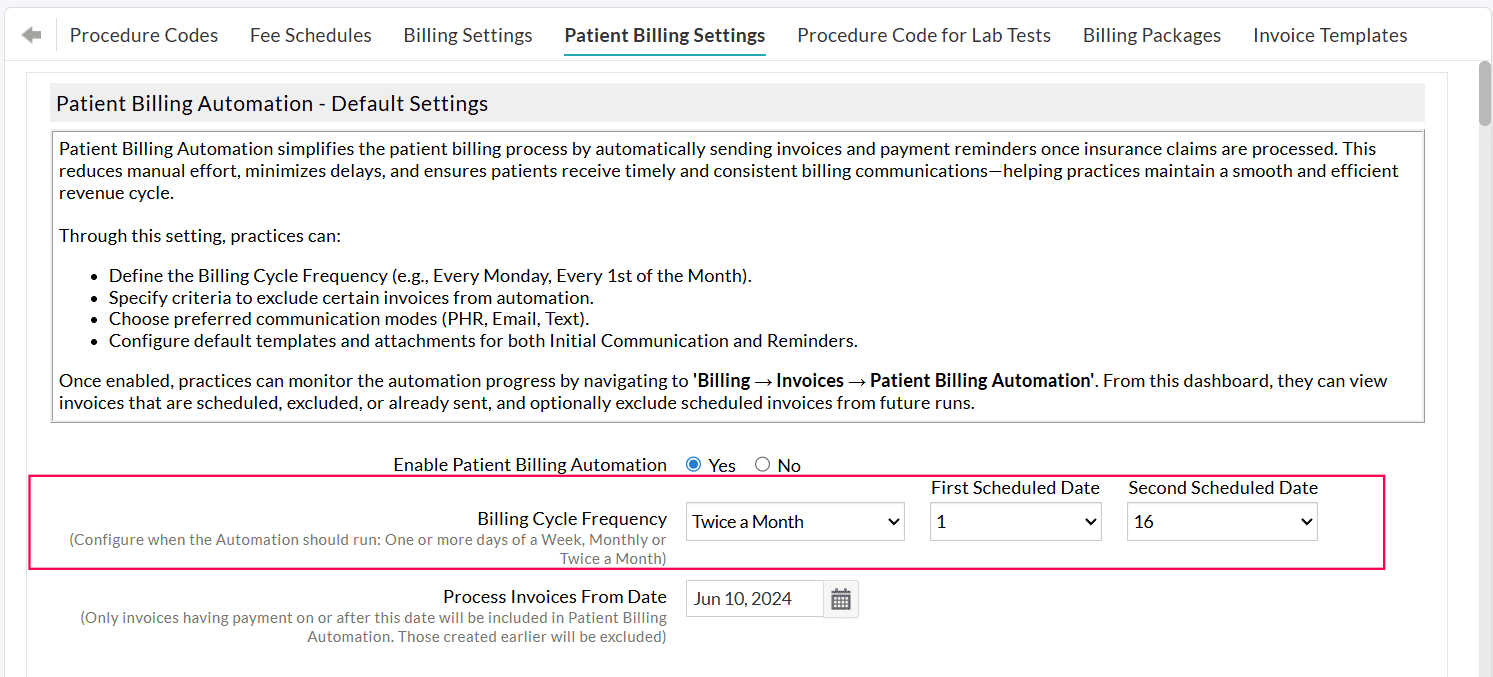
Configuring Billing Cycle Frequency
Choose how often Invoices should be sent automatically to the Patients. You can configure the automation to run on a Specific Days of a week, Monthly, or Twice-a-Month schedule based on your Practice’s billing workflow.
- Specific Days of a Week - Select one or more days of the week (e.g., Every Monday, Every Tuesday, Every Wednesday, etc.)
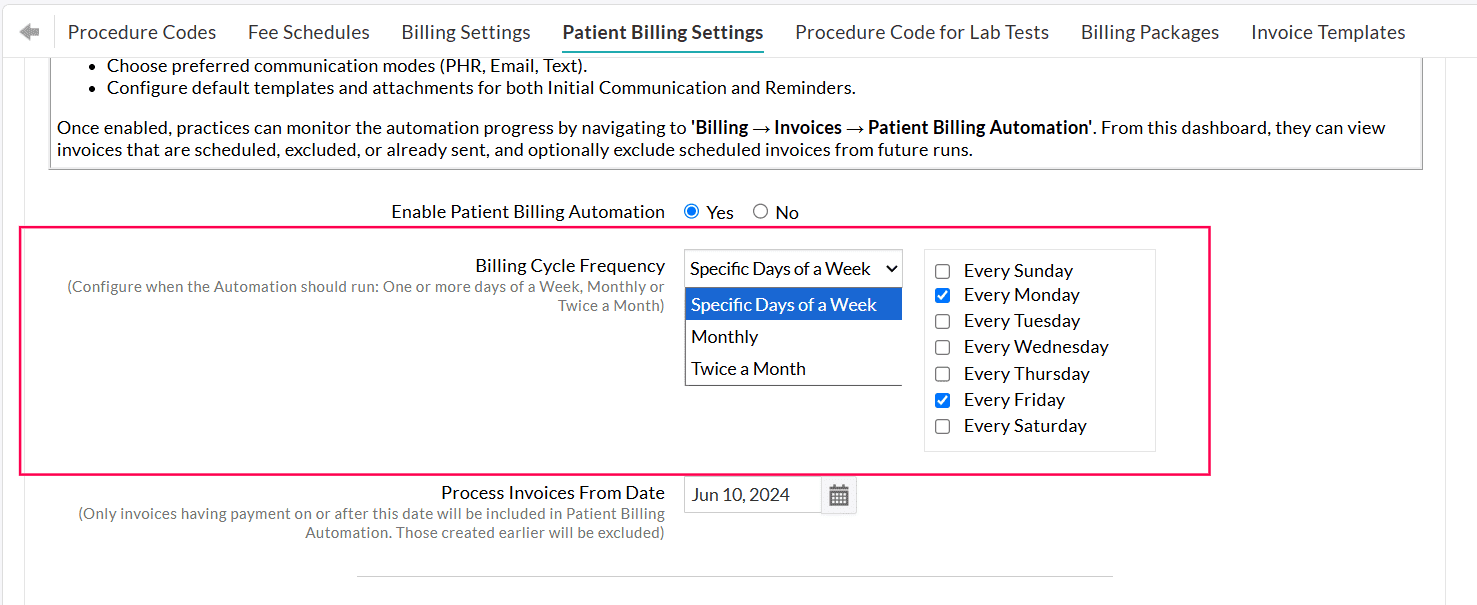
Example: If you select Specific Days of a Week → Every Friday, the system automatically sends all eligible Invoices to Patients every Friday. - Monthly - Select a specific date of the month (e.g., 1st or 15th of every month)
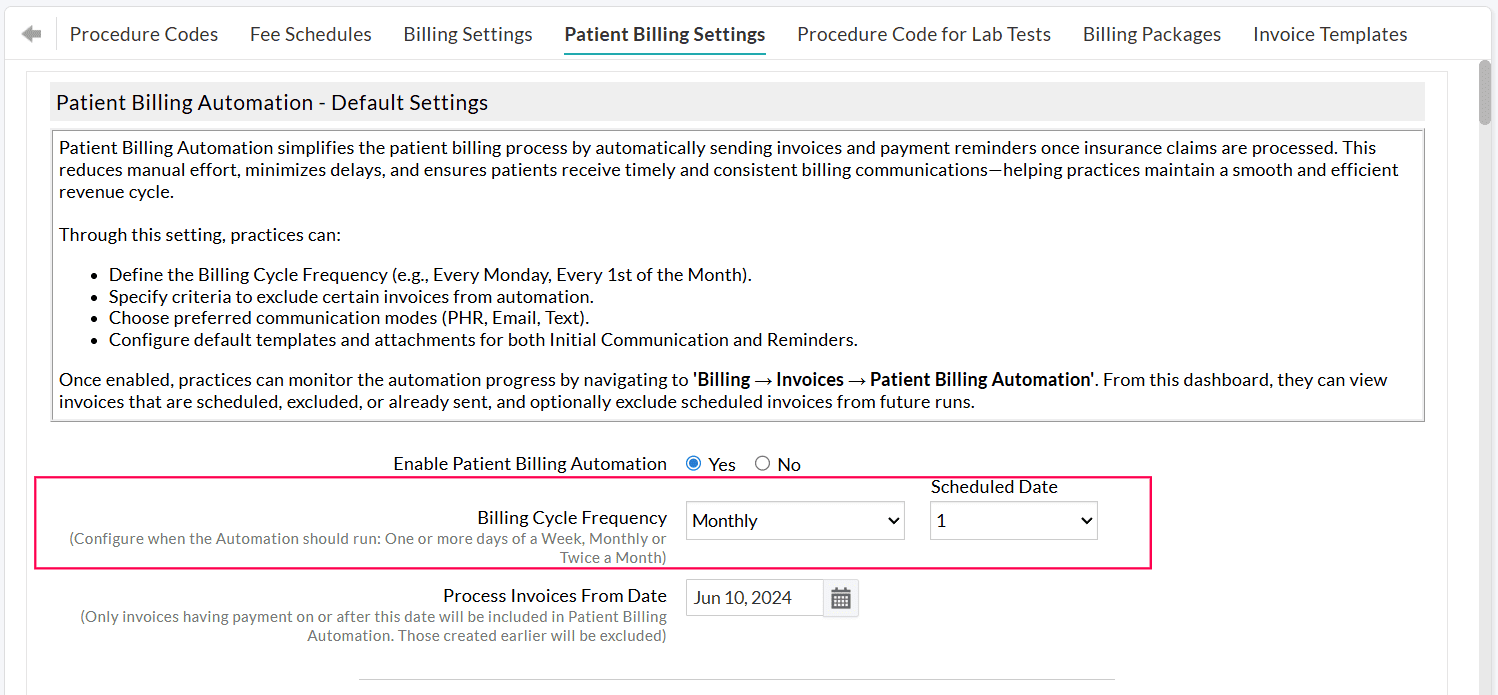
- Twice a Month - Choose two specific dates of every month (e.g., 1st and 16th of every month)
Process Invoice From Date
Set a start date to begin the automation. Only Invoices with payments posted on or after this date will be considered for automation.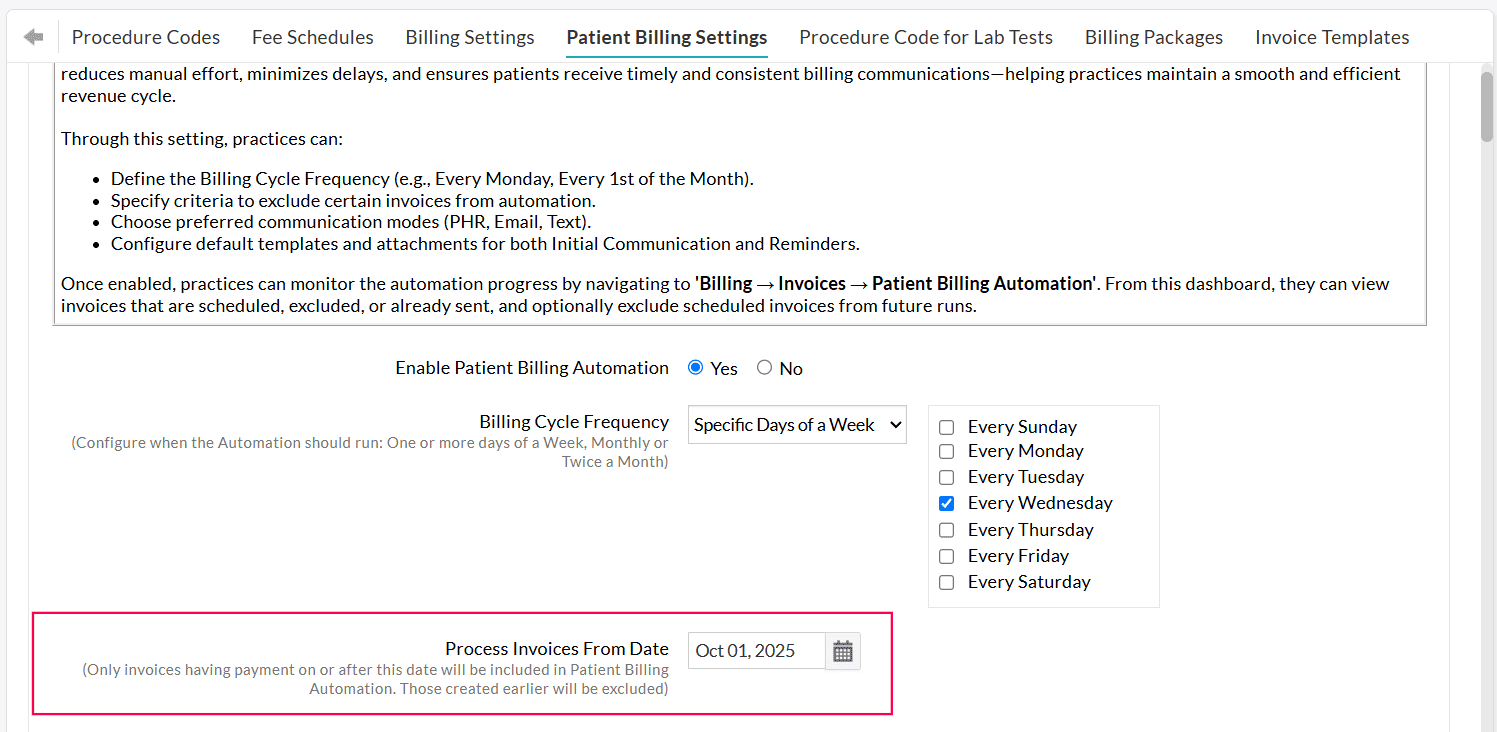
Enabling Automation for 'Initial Communication' and 'Reminders'
Practices can automate sending the first Invoice communication to Patients by navigating to 'Settings > Billing > Patient Billing Settings'.
Choose 'Yes' for 'Enable Sending Invoice Automatically'.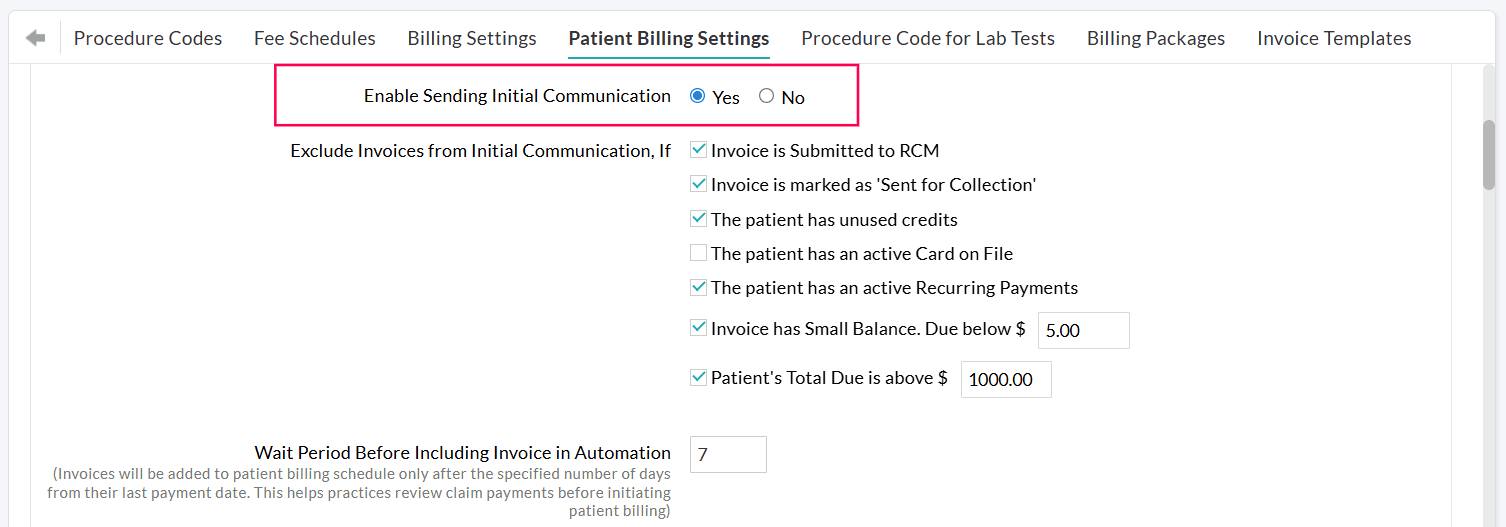
Practices can choose to automate only the initial communication while handling the reminders manually. Alternatively, they can send the initial communication manually and automate the reminders.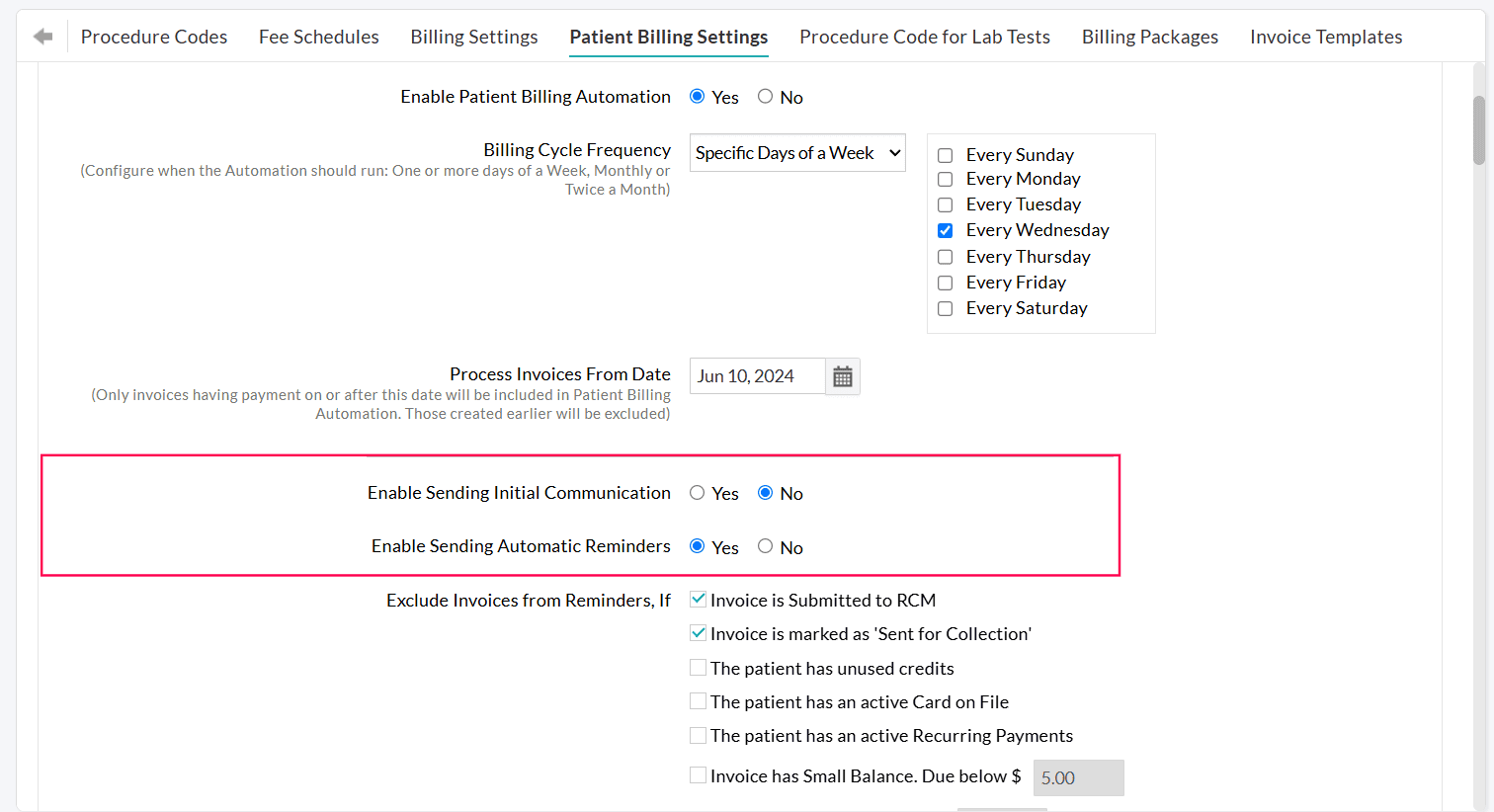
Excluding Invoices from Automatic Patient Billing
You can exclude Invoices from being sent automatically under the following conditions: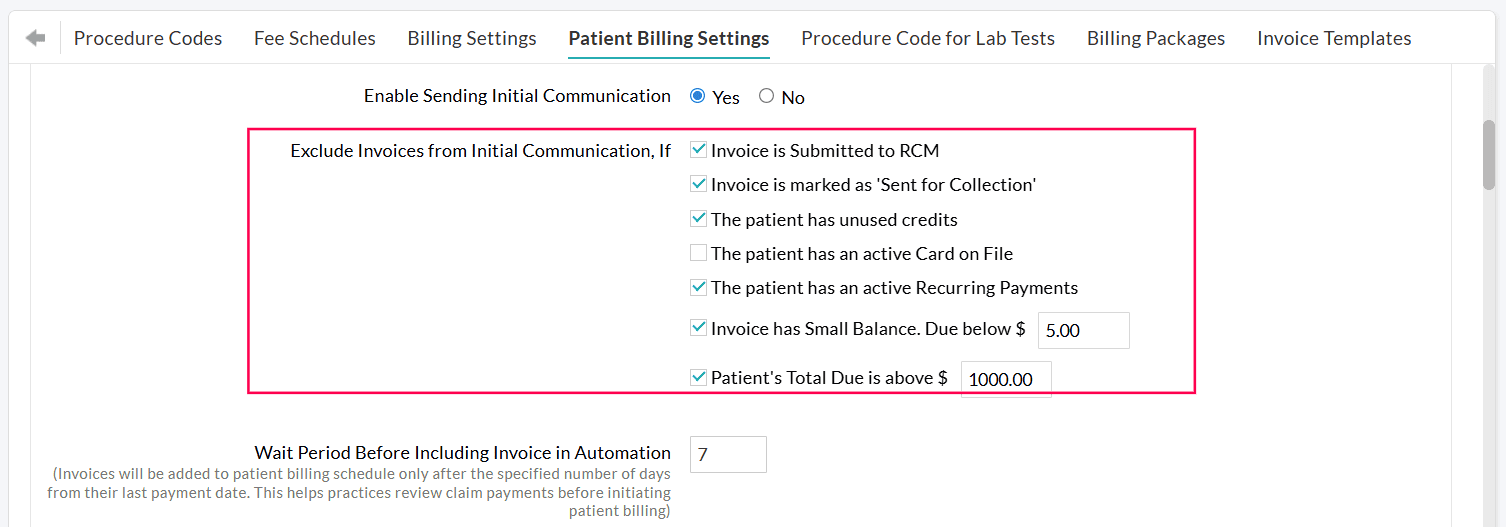
- Invoice is Submitted to RCM: This option is applicable for Practices that use Charm RCM or Charm BillerPro. Invoices submitted to RCM will be excluded from sending to Patients.
- Invoice is marked as 'Sent for Collection': Invoices sent to the collection agency will be excluded from sending to Patients.
- The Patient has unused credits: If the Patient has existing credits in their account, the Practice can apply these credits to clear outstanding Invoices. The Practice can exclude all Invoices of the Patient that have available credits. Once the Practice applies the unused credits to the Invoices, the remaining Invoices will be added to the automation.
- The Patient has an active Card on File: If a Patient has a card on file saved in CharmHealth, and the Practice has obtained consent to charge the Patient’s card, their outstanding dues can be cleared by processing the payment using the saved card. In such cases, Invoices for Patients with an active card on file can be excluded.
- The Patient has an active Recurring Payments: Practices that offer customized payment plans for Patients to settle their outstanding balances in manageable installments can enable this option.
- Invoice has a Small Balance: Invoices with a due below a configured limit (e.g., $5.00) can be excluded.
- Invoice Due is above a certain amount: Invoices with dues above the configured amount (e.g., $50) can be excluded. This allows Practices to verify high-value dues before sending them to the Patient.
- Patient's all Invoice Due is above a certain amount: If a Patient's total Invoice due exceeds the configured amount (e.g., $1,000), those Invoices can also be excluded.
Note: Practice must review all the excluded Invoices and send them manually if required.
Wait Period Before Including Invoice in Automation
Practices can configure the number of days the system should wait before an Invoice is scheduled for automation.
The Waiting Period will be applicable after the Claim payment is processed for the Invoice.
This helps Practices to:
- Review Claim payments and adjustments (All Invoices scheduled for sending will be listed under the 'Invoices > Patient Billing Automation' section.)
- Handle any special Patient Billing needs of some Patients.
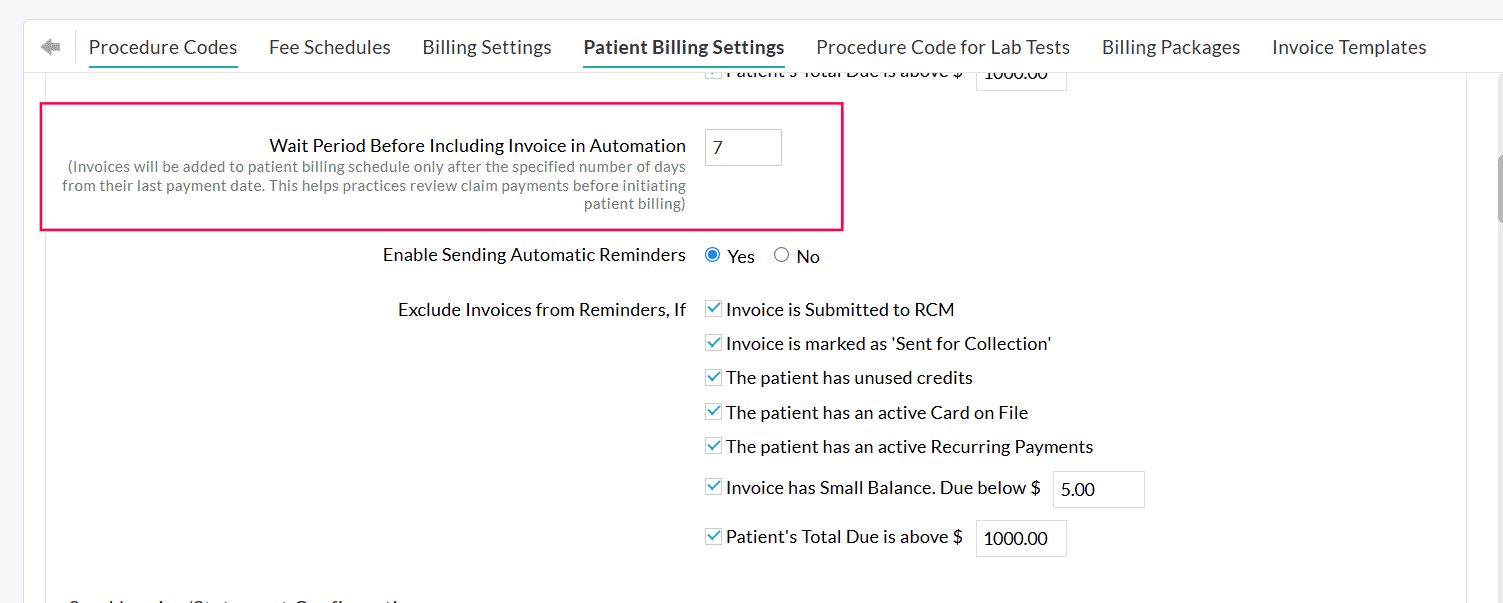
Example:
Configure a Wait Period of 7 days.
- The insurance payment is posted to an Invoice on October 10th.
- The 7-day waiting period begins. The Invoice will not be sent during this time. Practices can review the Invoice payments.
- On October 17th, the waiting period ends. The Invoice will be sent to the Patient automatically on your next scheduled billing cycle.
Note: If the Claim is resubmitted before the wait period ends, the Invoice will be automatically excluded from the automation.
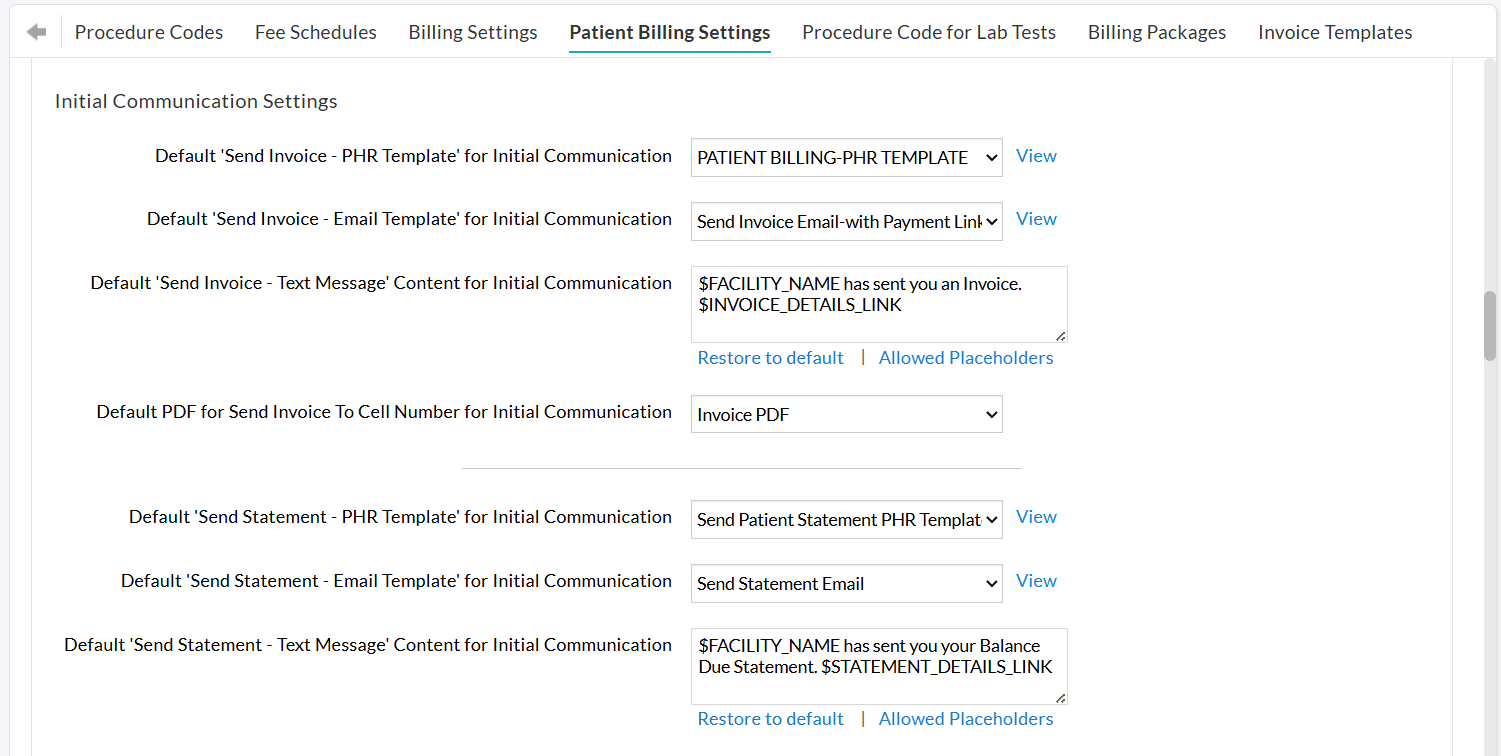
Configuring Initial Communication Settings
- Choose the default communication modes to send Invoices or Statements to Patients, viz., PHR, Email, and Text Message.
- Send Invoices as a Statement when the Patient has multiple Invoices.
If a Patient has more than one outstanding Invoice, you can enable the 'Send as Statement' option to combine and send them as a single statement. - Include 'Payment Link' while sending Invoices.
If the Bluefin Payment Gateway is enabled for your Practice, you can include a payment link in the Invoice message for Patients to make payments and select the default beneficiary for each Facility to which the amount should be credited. - Select default templates for sending Invoices and Statements through different communication modes, viz., PHR, Email, and Text Message (Cell Number).
Configuring Automation for Reminders
After the initial Invoice is sent, you can also automate follow-up reminders to Patients who still have outstanding dues.
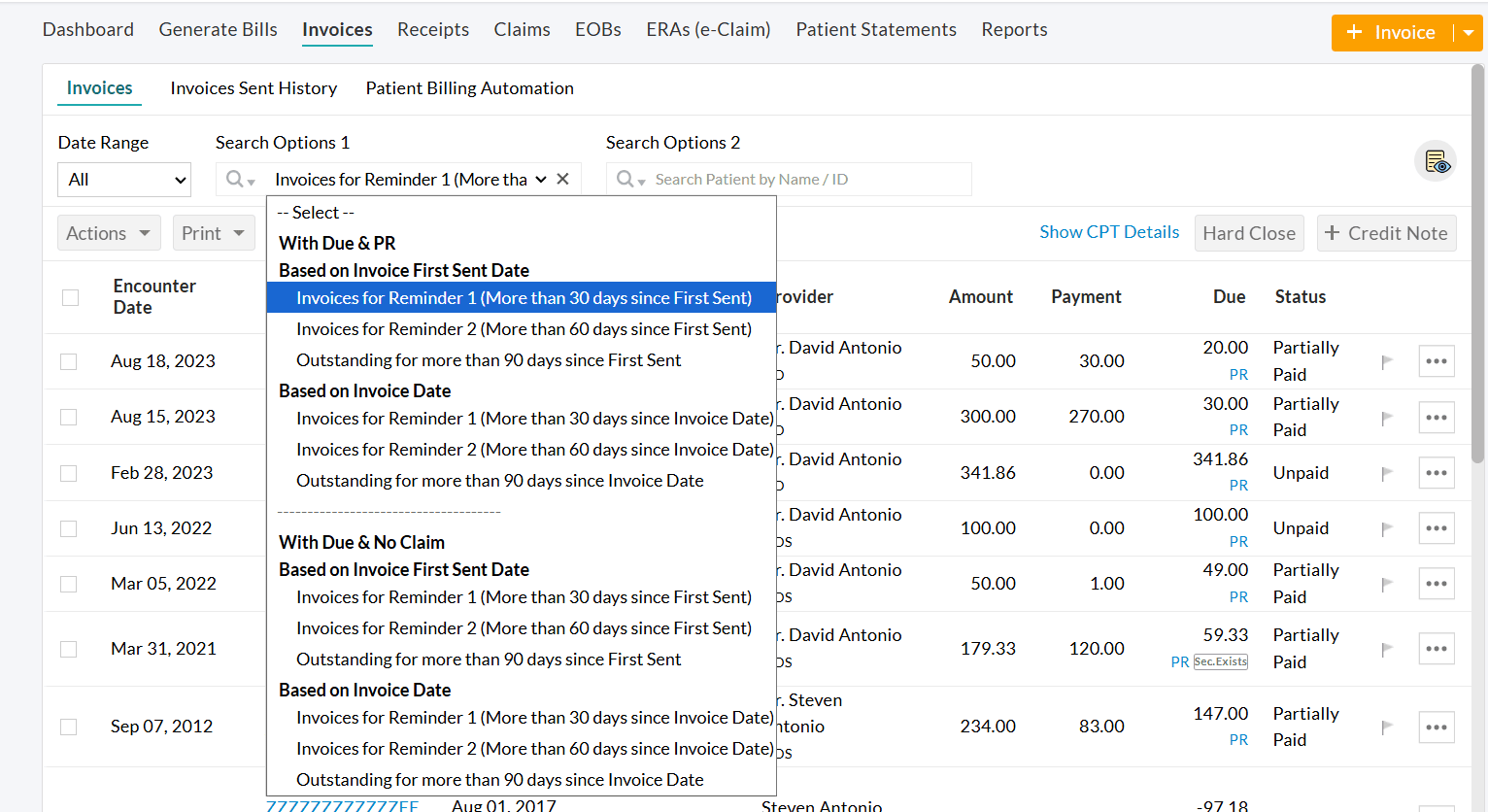
Invoices located within 'Billing > Invoices > Search Options 1 > Patient Billing - Reminders' are eligible for sending automated reminders.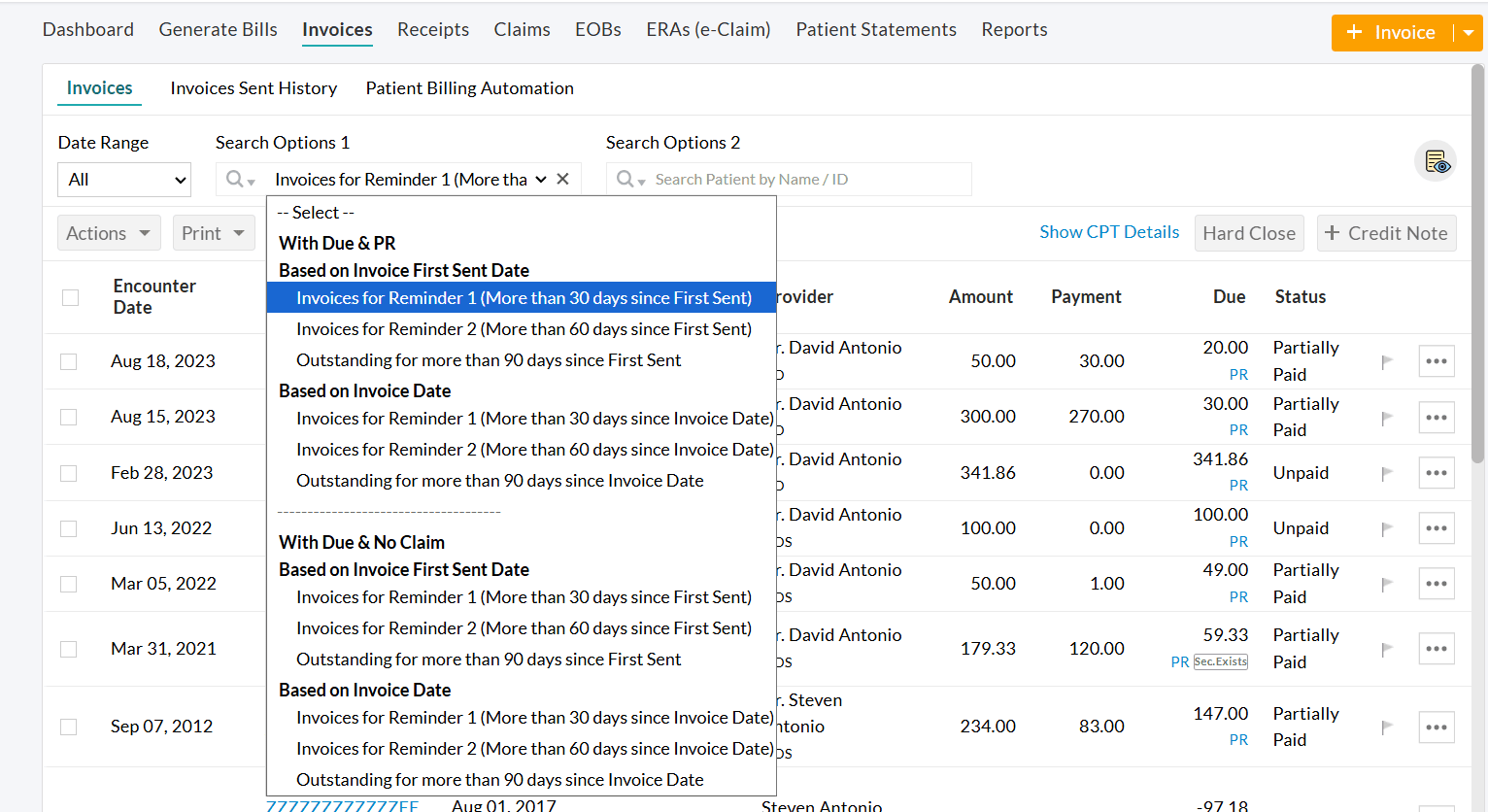
To enable this feature,
- Navigate to 'Settings > Billing > Patient Billing Settings'.
- Choose 'Yes' for 'Enable Sending Automatic reminders to Patients'.
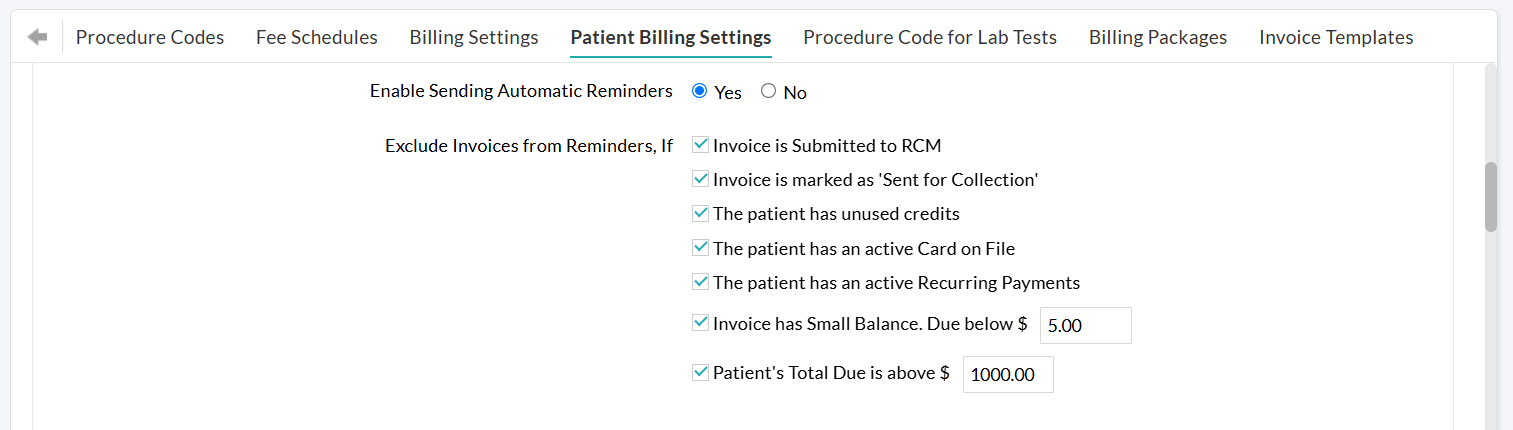
You can configure separate exclusion criteria for reminders, similar to the initial communication.
For example, you can choose not to send reminders for Invoices that are already submitted to RCM, sent for collection, or have small balances, etc.
Configuring Reminder Settings
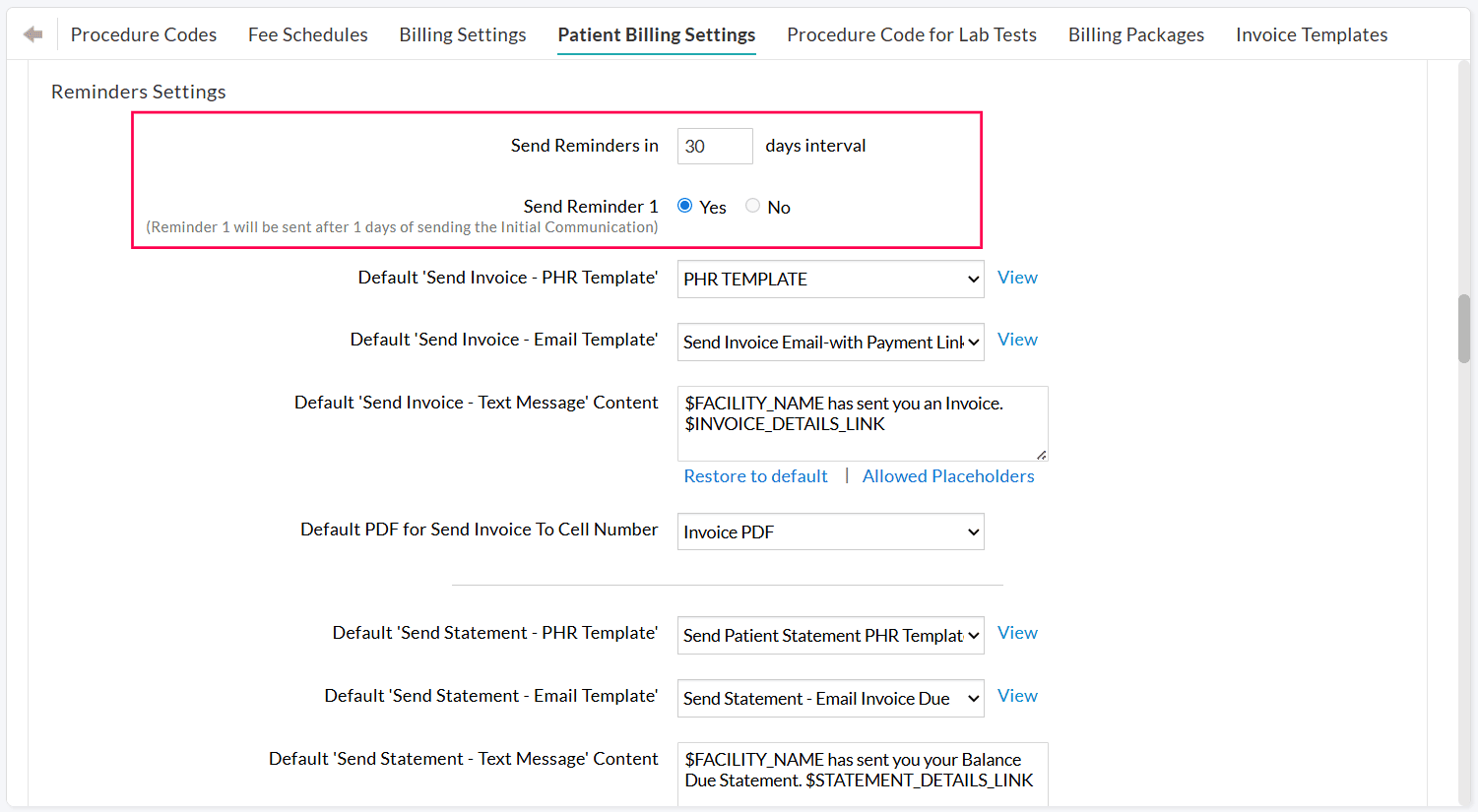
Practices can use this section to define:
- How often should reminders be sent to the Patients
- How many reminders should be sent. You can send up to three reminders for each Invoice after the initial communication.
Example:
If the reminder frequency is set to every 30 days, and the initial Invoice is sent on March 1,
- Reminder 1: Sent on March 31 (30 days after the first Invoice).
- Reminder 2: Sent on April 30 (60 days after the first Invoice and 'Reminder 1' is sent).
- Reminder 3: Sent on May 30 (90 days after the Invoice and 'Reminder 1' and 'Reminder 2' are sent).
Note: The configured reminder frequency and schedule will be applied while sending Invoices from 'Billing > Invoices > Search Options 1 > Patient Billing - Reminders'.
Practices can customize default templates for each reminder ('Reminder 1', 'Reminder 2', and 'Reminder 3') based on the chosen communication mode(s).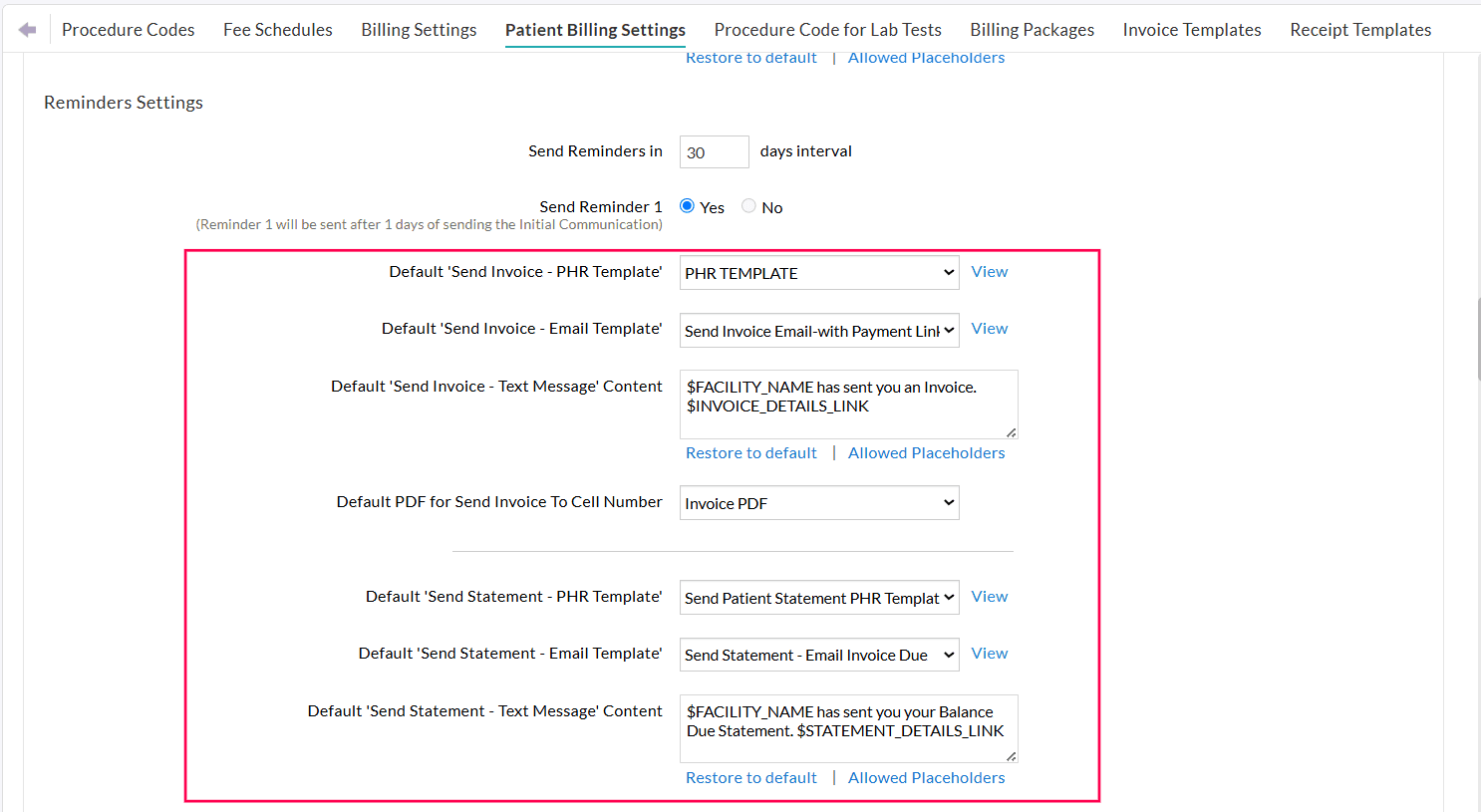
If 'Reminder 3' is enabled, Practices can choose to continue sending reminders to Patients at the configured interval even after the third reminder, as long as the Invoice still has an outstanding balance.
For example, after Reminder 3 is sent, additional reminders will be automatically triggered every 30 days until the Invoice is fully paid.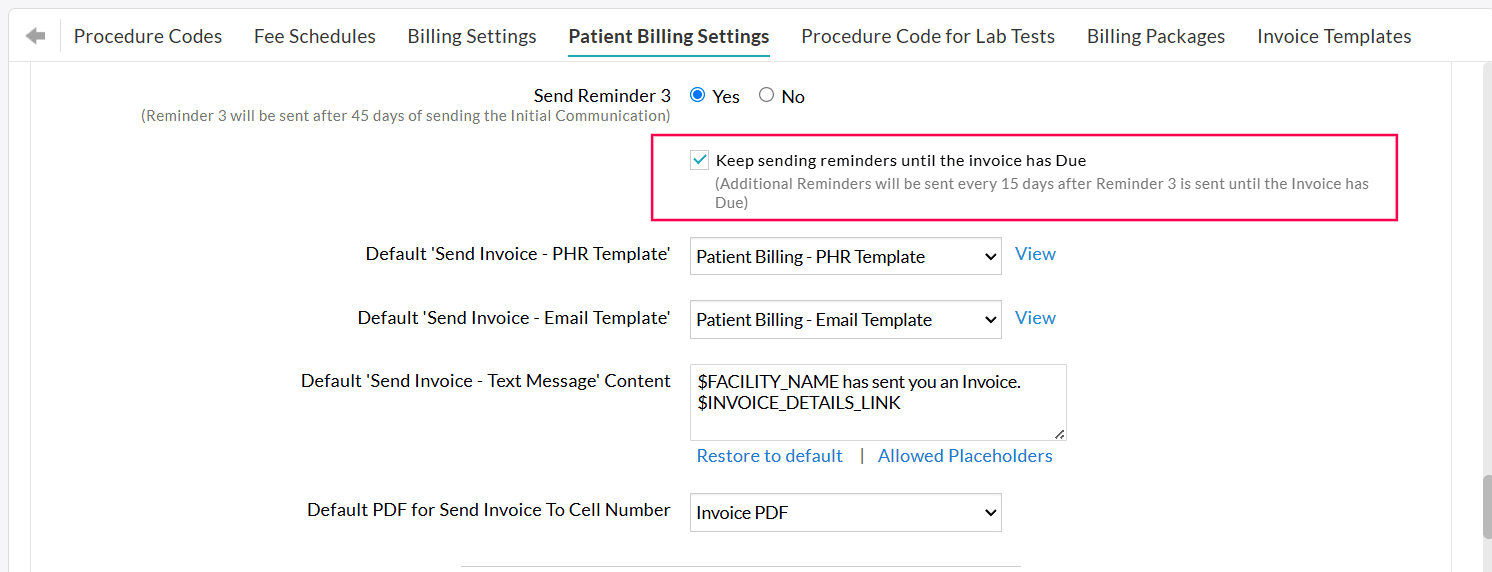
Handling Invoices Not Paid After Three Reminders
Invoices that remain unpaid even after three reminder notifications are listed under 'Billing > Invoices > Search Options 1 > Patient Billing – Reminders > Outstanding for more than 90 days since first sent.'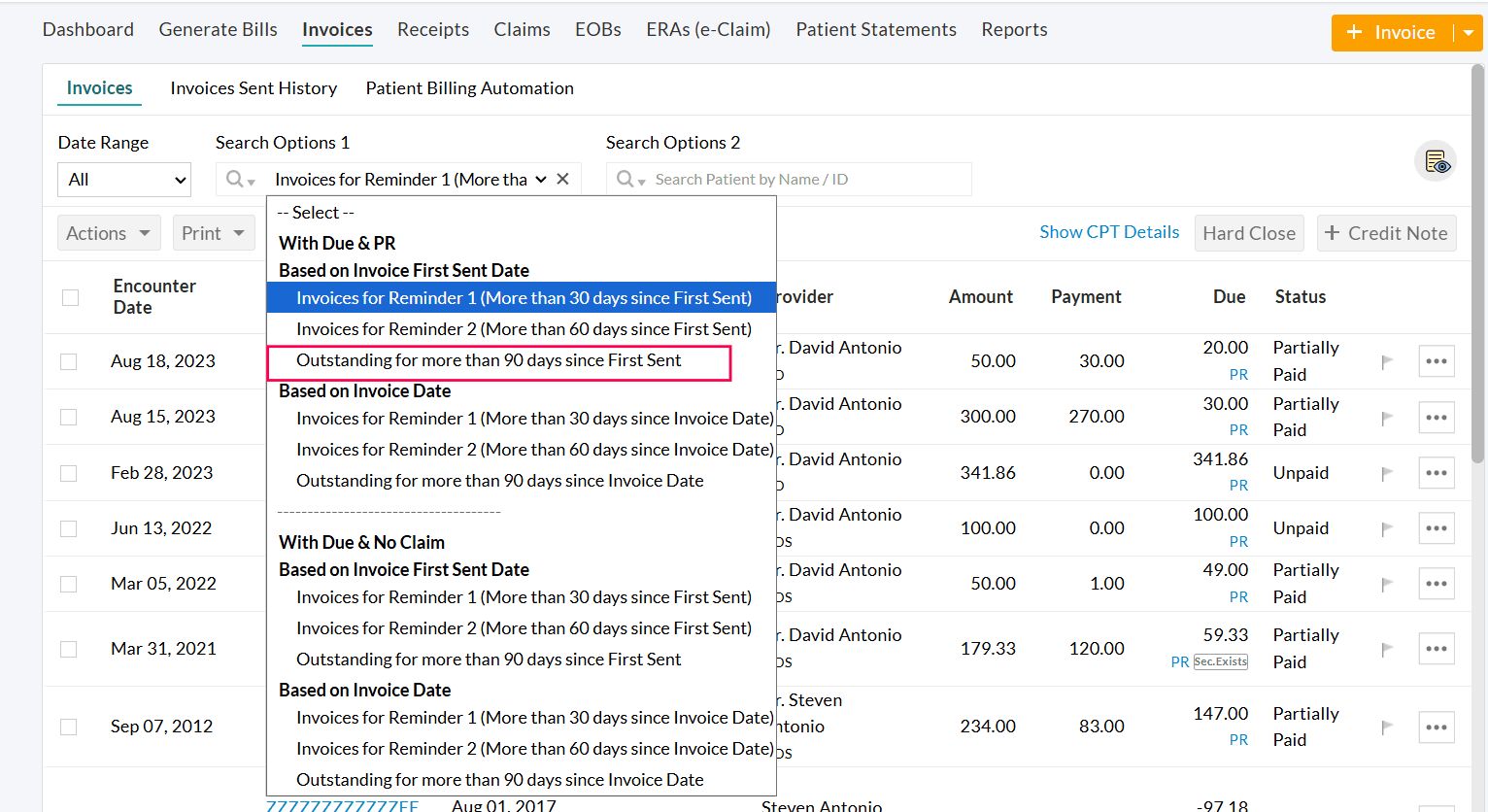
To collect these outstanding balances, Practices can take the following actions based on the Practice policy:
- Send Invoices to Patients by mail.
- Send Invoices to a Collection Agency for further payment follow-up.
- Reach out to Patients directly and offer customized payment plans, allowing them to clear their dues.
Tracking the Patient Billing Automation Progress
You can monitor and manage all automated billing activities from 'Billing > Invoices > Patient Billing Automation.'
This dashboard offers a clear overview of scheduled, excluded, and send Invoices. Additionally, it enables you to exclude scheduled Invoices from future automation runs manually.
To help you quickly locate specific Invoices, this page includes a custom date-range filter and detailed Search Options.![]()
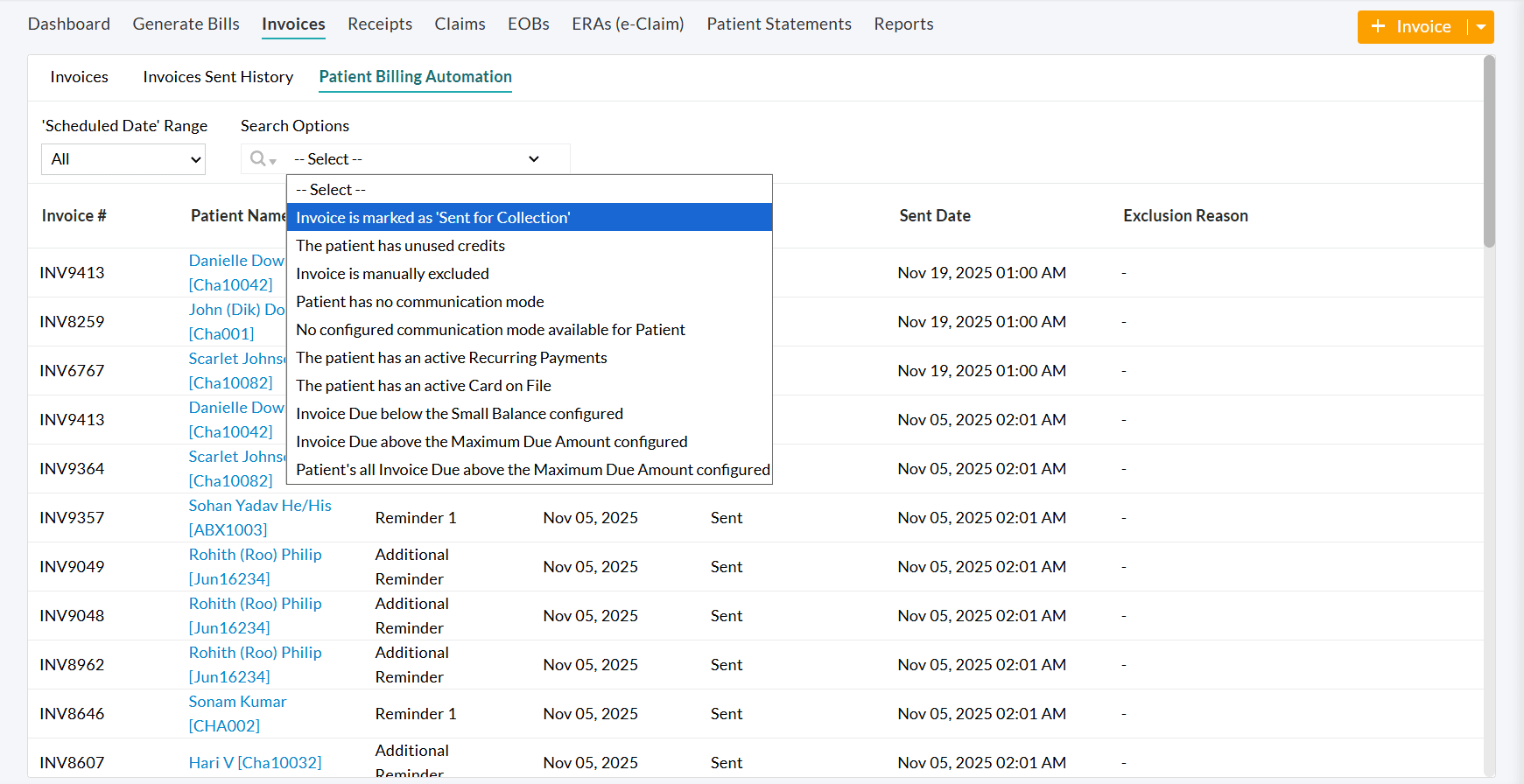
The Search Options include:
- Invoice Number - Find an Invoice using its reference number.
- Initial Communication/Reminders - Search Invoices based on their communication status, such as:
- Initial Communication
- Reminder 1
- Reminder 2
- Reminder 3
- Additional Reminder
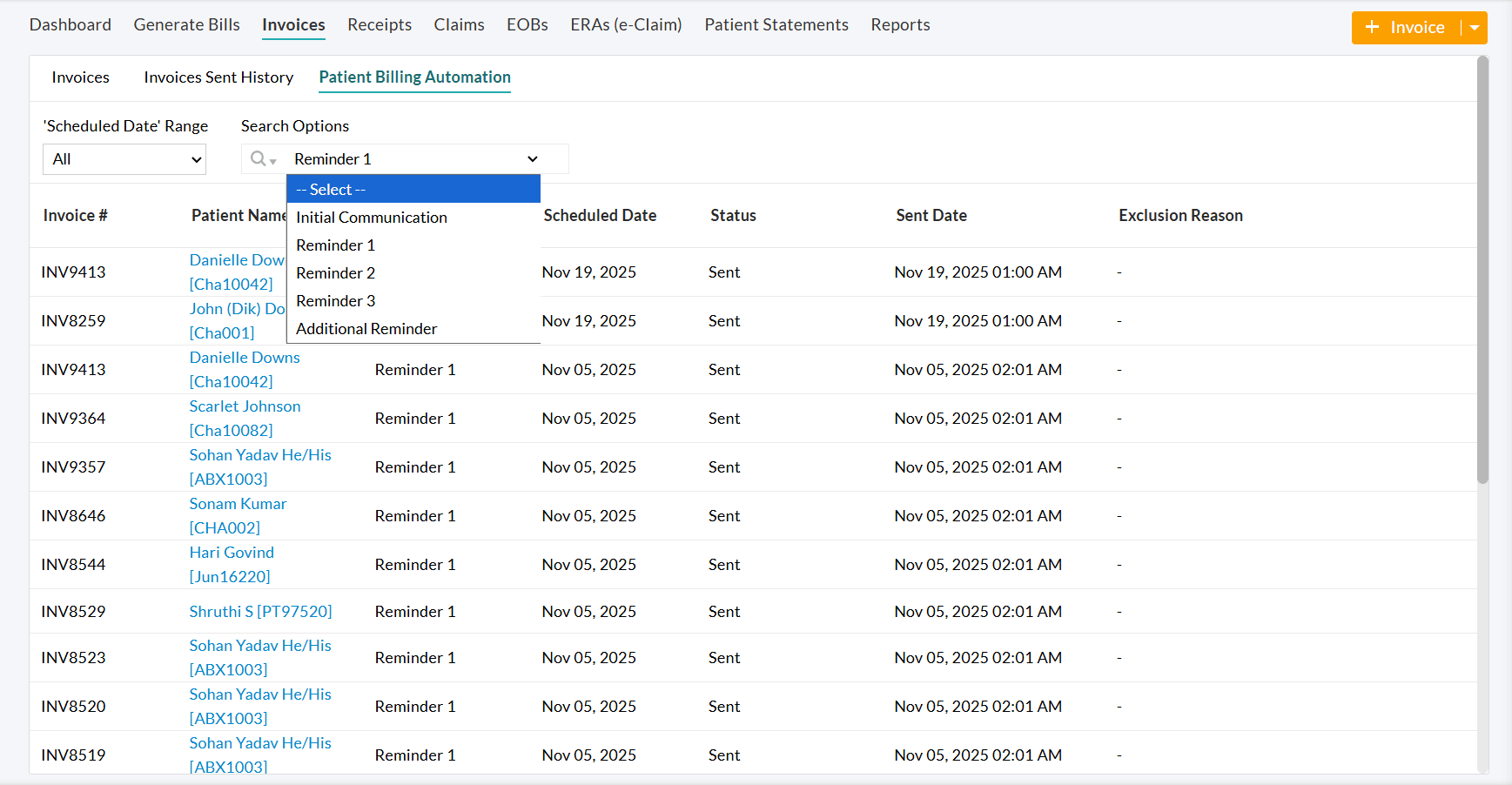
- Status - Filter Invoices based on their current automation status.
- Exclusion Reason - View Invoices based on the reasons for their exclusion.