Dashboard and Reports
RCM Dashboard
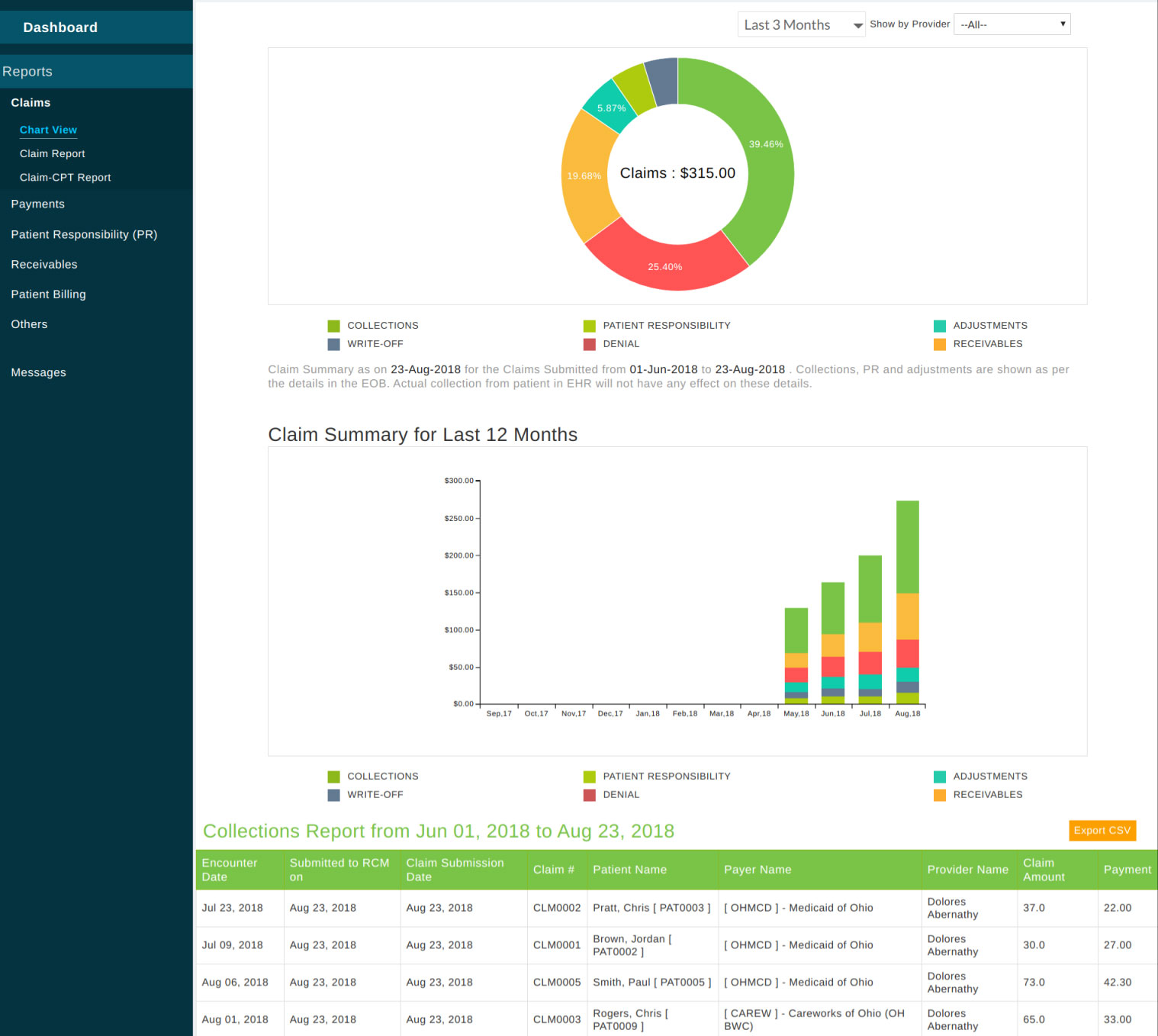
The Dashboard view gives a summary of claims submitted to the payer. It shows the consolidated amount of Claims submitted, Collections received from payers, Patient Responsibility, Adjustments, Write-offs, and Denial in the selected date range. Generally, insurance companies pay only the allowed amount for the CPT. Payments, adjustments, patient responsibility are applied on claims as given in Explanation of Benefits (EOB).
Claims - It is the total claim amount submitted to the payer.
Collections - It indicates the total payment collected from the payer for the claims.
Patient Responsibility - When EOB has Patient Responsibility such as co-pay, co-insurance, deductible, etc. are posted to procedures in the claim. If necessary, this can be invoiced to the patient by the practice. Here the sum of Patient Responsibility in claims is shown.
Adjustments - Difference between CPT charge and allowed amount from EOB will be marked as Adjustment. Here the sum of adjustment in claims is shown for the selected date range.
Write-off - It is generally given on providers' requests to a claim and not given from RCM. It is not related to the Write-offs in EHR.
Denial - When CPT payment is not received from payer even after appealing, the CPT is marked as denied. This indicates the sum of the denial amount in the claims. Receivable indicates total claim due as on the report date. It is the sum of the claim amount for which payment is awaited.
On clicking the respective amount link in the info-graphic, itemized reports are shown at the bottom.
The last 12 months claim report is shown as a graph. This graph represents the month -wise data on the amount submitted to claims, collected from payers, patient responsibility, adjustments, denial, and write-off. Receivables represent the outstanding amount at the end of the respective month. Hovering the mouse over it shows further details. The reports can also be filtered by the provider.

The menu on the left shows various reports available. All the reports can be exported as a CSV file.
Claim
Chart View - The claim summary can be seen on clicking the 'Chart View' link under Claims (below Dashboard link) on the left side menu. The donut chart gives details of claims generated in the selected date range. On clicking the section of the donut chart, the respective report is shown at the bottom of the page. The stacked bar chart indicates a claims summary for the last 12 months.
Reports
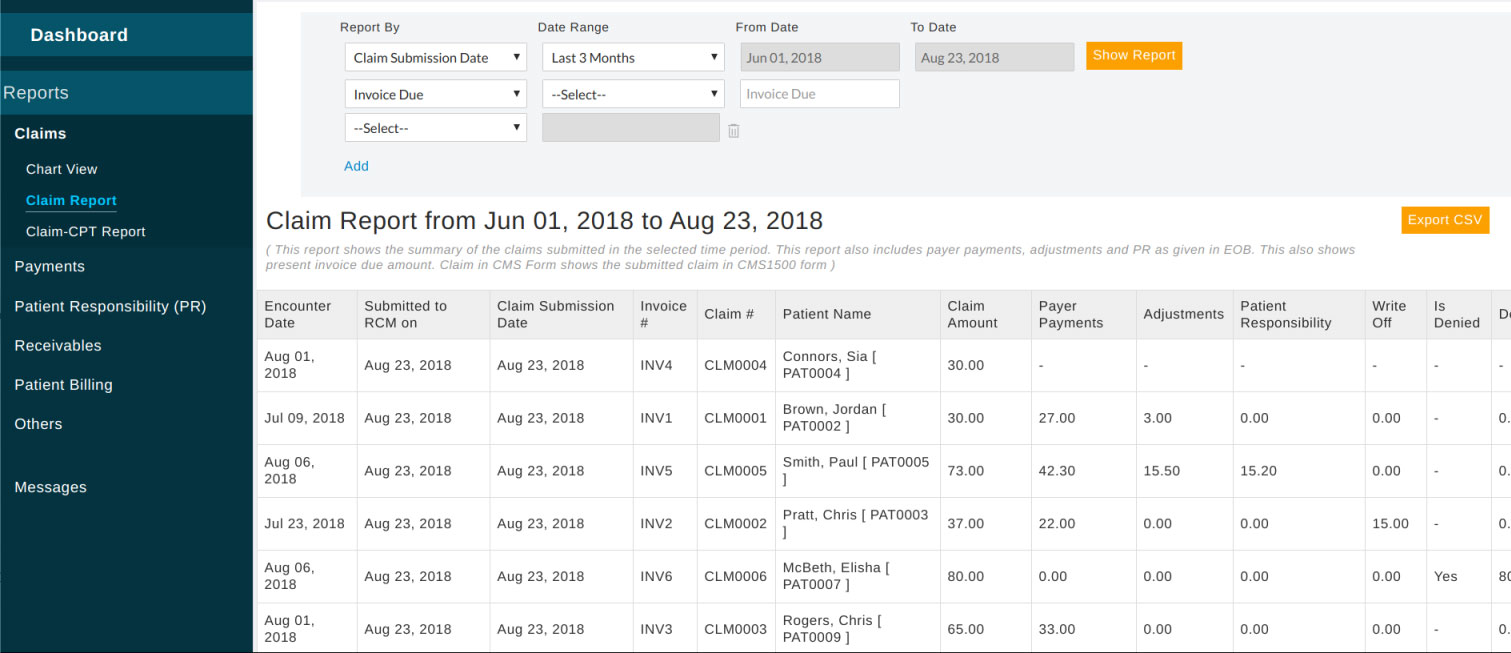
Claim Report - This report shows details of the claim such as payments, adjustments, denials, patient responsibility, etc. It can be further filtered with multiple criteria like provider, patient, payer, status, etc.
Claim-CPT Report - This report shows all the claims submitted with the CPT details
Payments
Payment Report - This report shows payments of claims in the selected payment date range. It can be further filtered with multiple criteria like provider, patient, payer, reference number, etc.
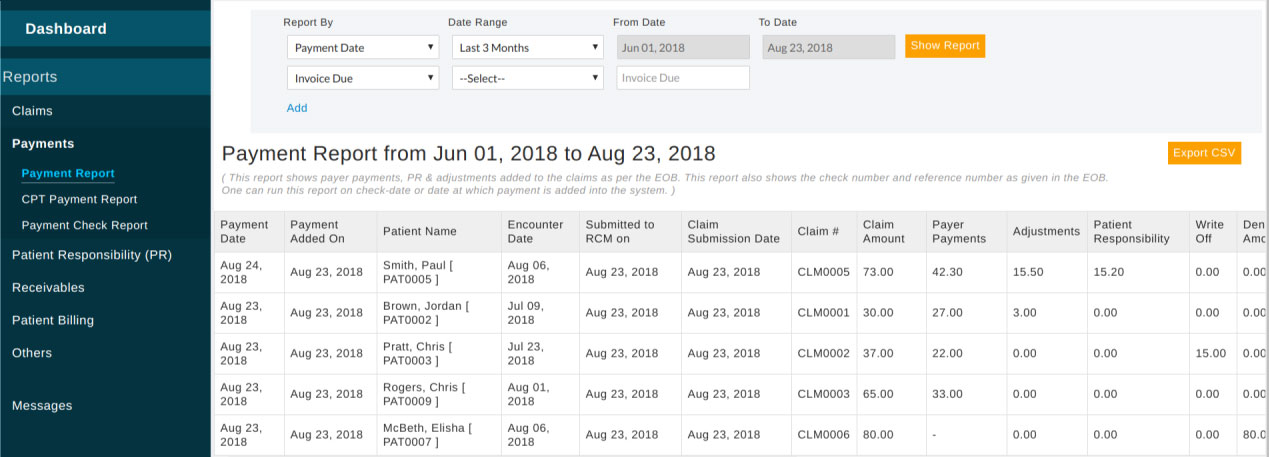
CPT Payment Report - This report shows payments collected against each procedure (CPT code) in the claim.
Payment Check Report - It is a report for a check received from the payer in a specified date range.
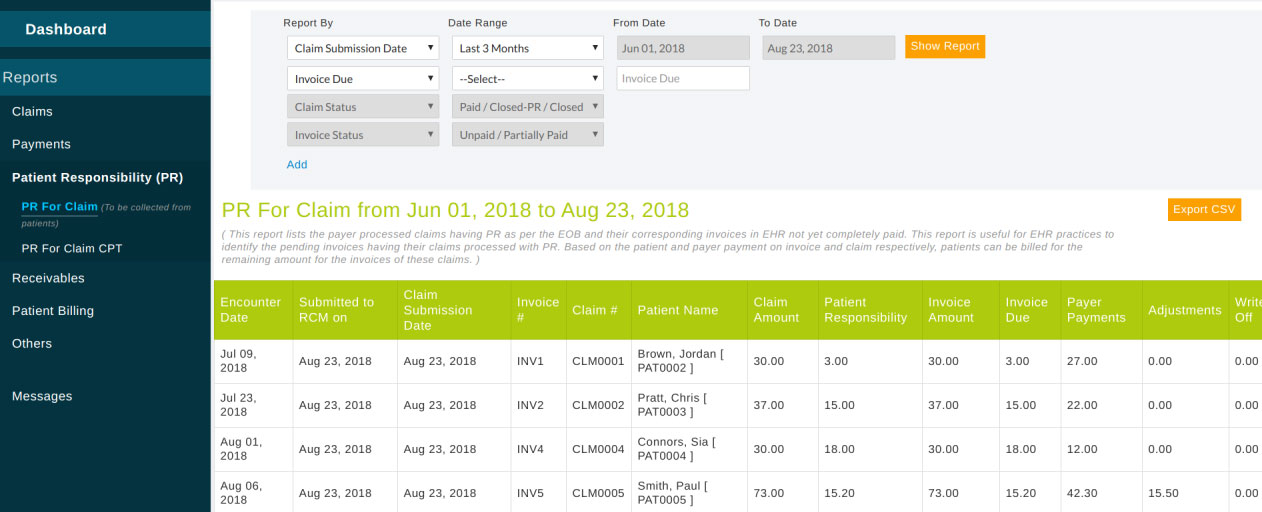
Patient Responsibility Report
This report shows patient responsibility details of the claims. Reports can be filtered on the type of responsibility too.
Receivables
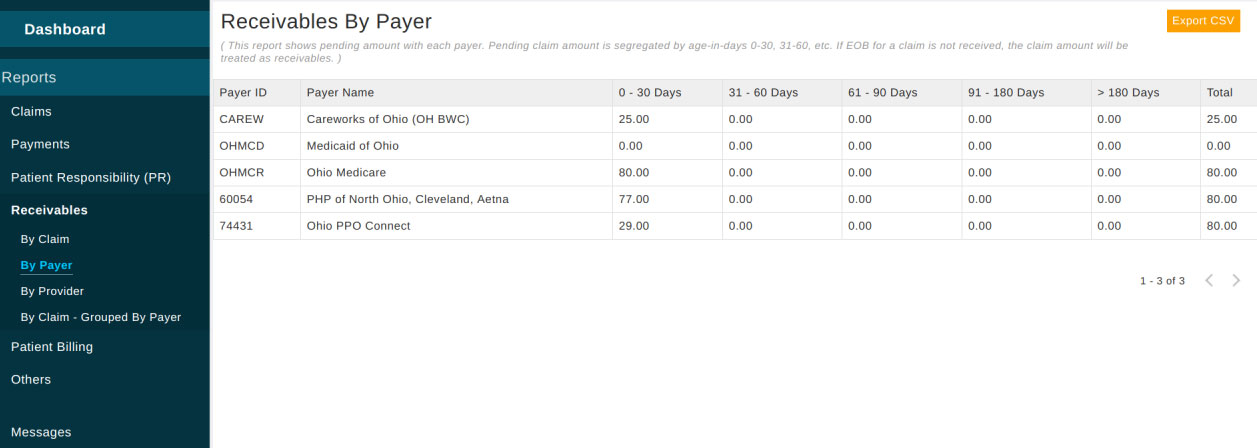
By Claim - This report can be used to pull the outstanding claims and their age in days. Payer wise report with outstanding claims can be pulled in using the option 'By Claim - Grouped By Payer.
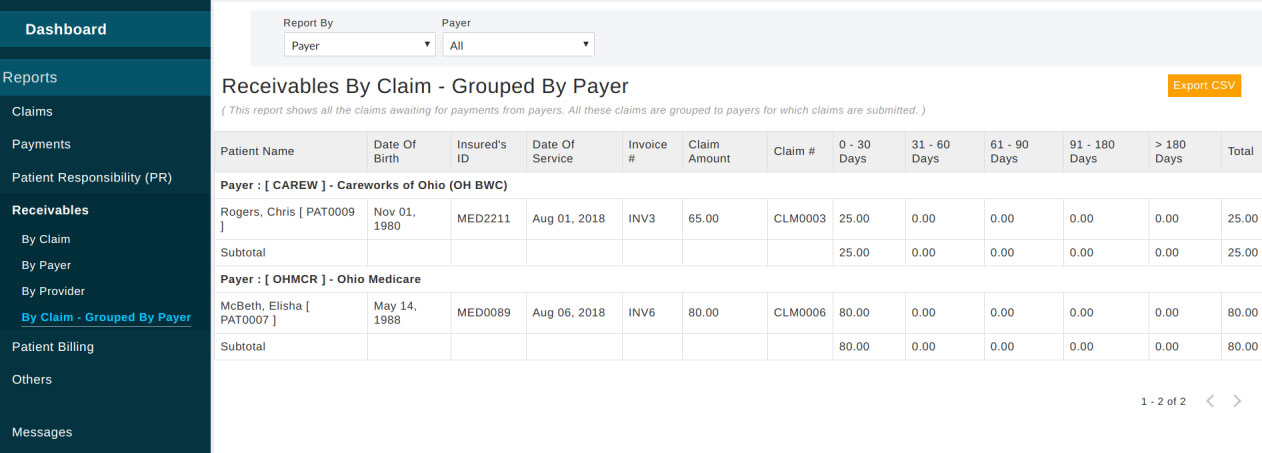
Receivables 'By Payer' and 'By Provider' can be pulled by clicking respective links available under 'Receivables'.
Patient Billing
Patient Bills Sent Report - It lists the chart invoices mailed, emailed or sent to the patient portal (PHR) account.
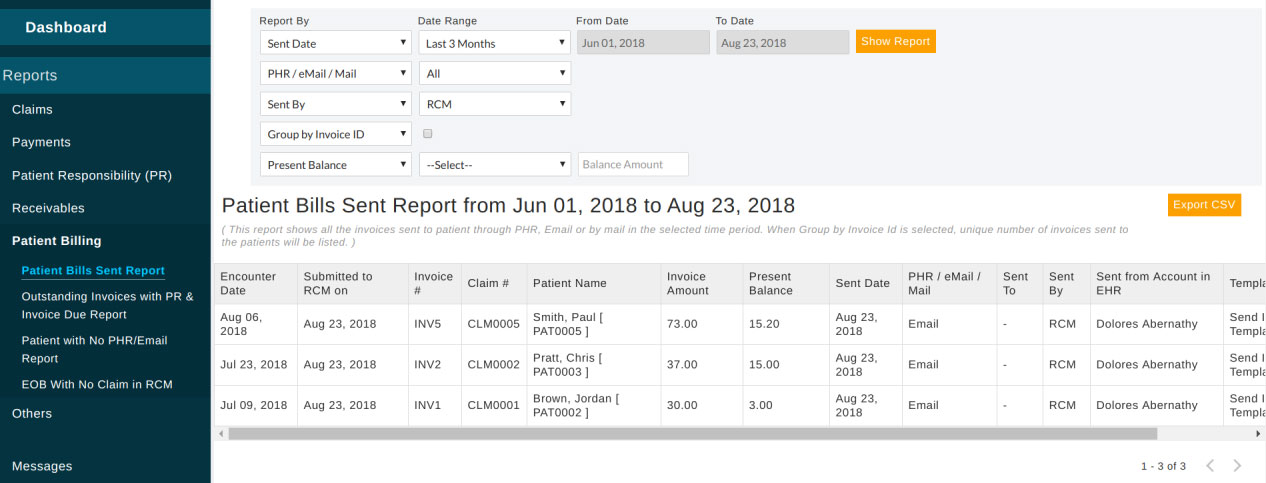
Outstanding Invoices with PR & Invoice Due Report - This report shows the outstanding invoices with patient responsibility.
Patient with No PHR / Email Report - This lists the patients without a personal email address and patient portal (PHR) account.
EOB With No Claim in RCM - Lists EOBs received which have no claims sent from RCM service. Maybe these are EOBs for claims sent from EHR practice earlier.
Others
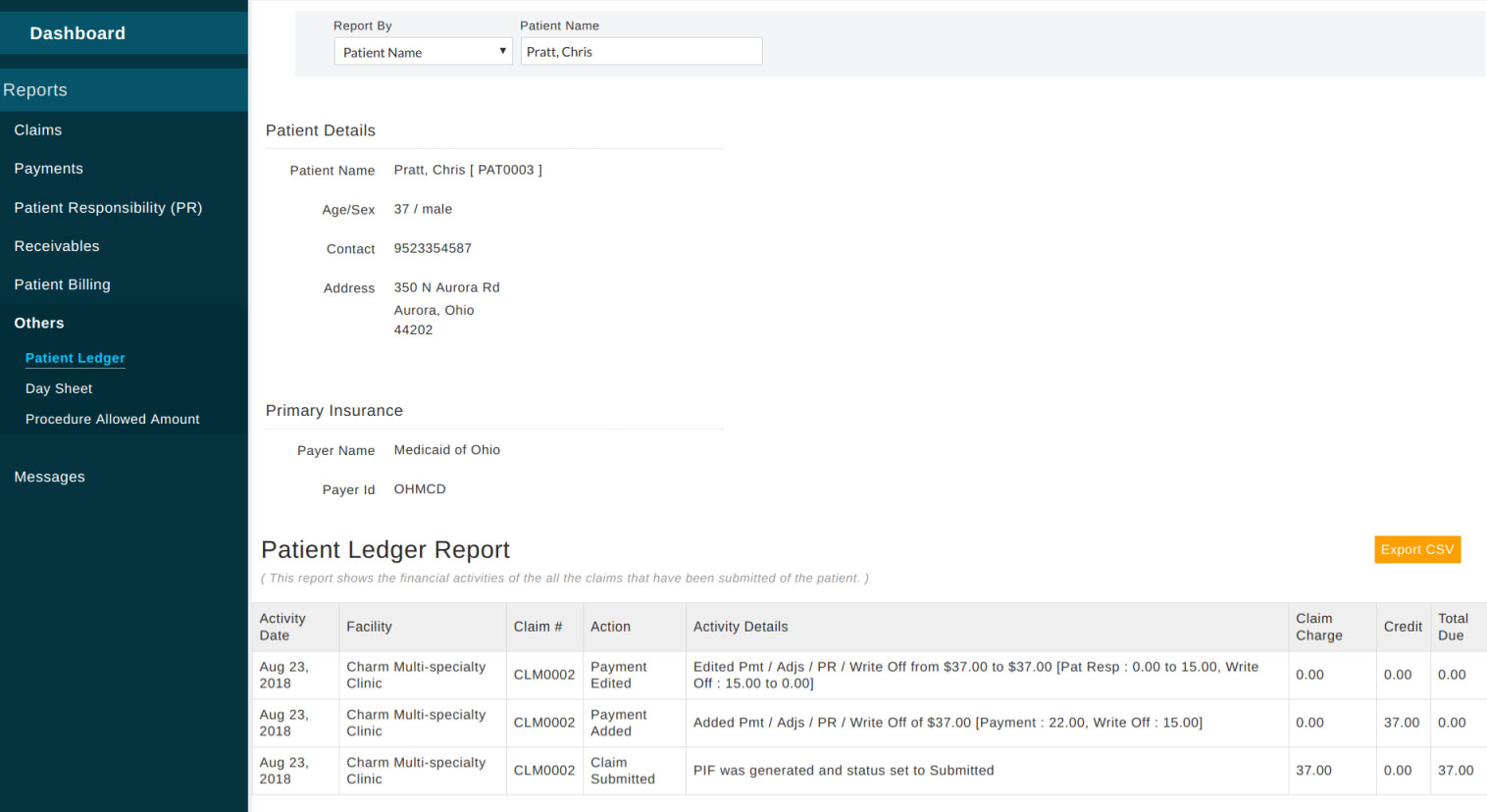
Patient Ledger - Shows ledger of a particular patient.
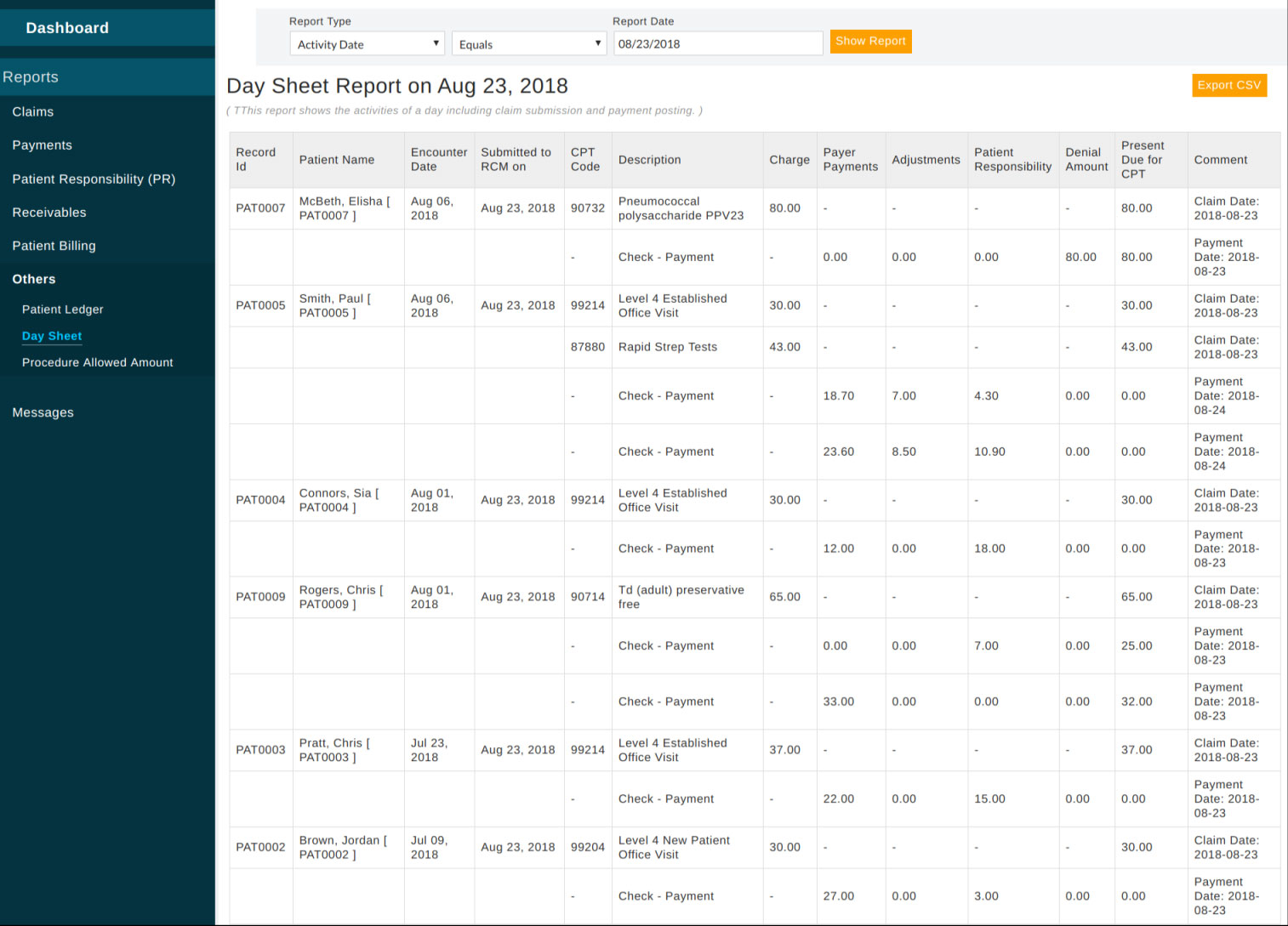
Day Sheet - Shows claim related activity on any selected date.
RCM Service Invoicing
RCM service invoice report on the dashboard is used to invoice the practice for the service rendered to the practice. RCM service charge is a specific percentage(%) of the collection amount. Depending on the RCM contract you have with the practice, necessary patient responsibility can also be a part of the collection.
As a part of Patient Billing, EHR invoices mailed to the patient on behalf of the practice and marked as mailed using the 'Mark as Mailed' option can also be included in the Service Invoice Amount.

If this invoice is sent to the practice, use "Mark as Invoiced". When it is marked as invoiced, these collections will not show up again for the next RCM service invoice.
This report is only visible to privileged members which can be managed in Admin Settings → Member List → Member Privileges.