Information for Practices
Submitting Charts/Invoices to RCM
A completed chart can be submitted to RCM from the Billing section of EHR either from
- Generate Bills
- Invoices
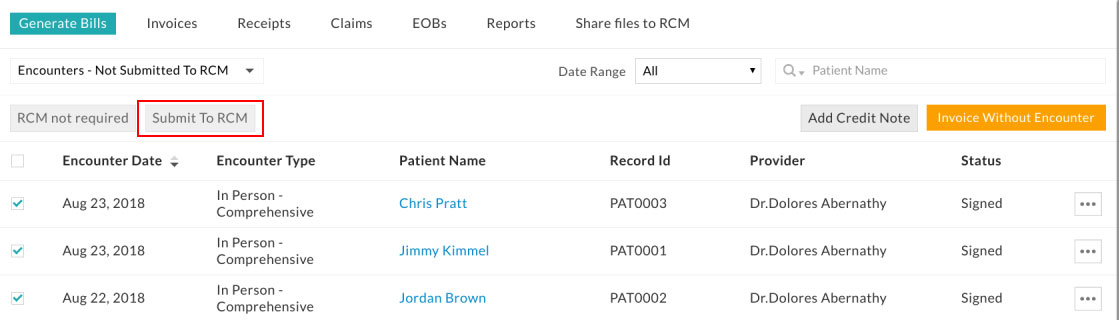
In the Generate Bills tab, all the encounters of the practice will be listed. These encounters can be submitted to RCM for claim processing by using the 'Submit to RCM' option.
Refer to the screenshot below.

More than one encounters can be submitted at a time by clicking the 'Submit to RCM' button on the top. An invoice will be created for encounter upon submitting to RCM with the invoice amount as procedure total.
When the claim is not required for an encounter, it can be marked as 'RCM not required'.
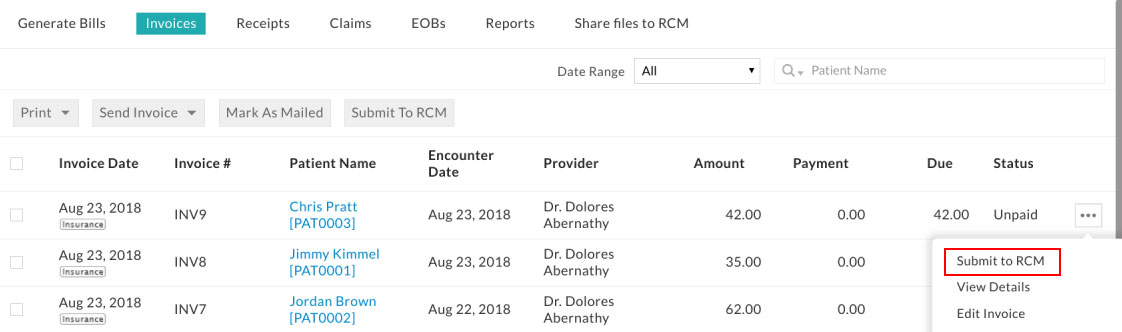
When an invoice is already created for an encounter, it can be submitted to RCM from the Invoices tab by using the 'Submit to RCM ' option as shown below. Submitted invoices will be marked with RCM Tag.
Details required to submit Charts/Invoices to RCM
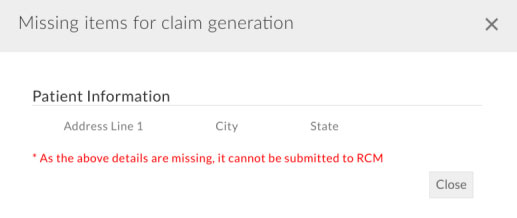
For submitting Charts/Invoices to RCM, the following information is required
- Patient Demographics (patient address and contact number)
- Patient's Insurance Information (payer details, insurance id)
- Treatment Information (procedure and its related diagnosis codes)
When submitting Charts/Invoices to RCM, the user will be prompted to provide the missing information required for claim generation. Refer to the below screenshot.
Secure Messaging with RCM Team
Claims submitted to insurance companies and their status can be tracked in RCM Dashboard by logging into https://rcm.charmtracker.com with EHR user credentials. Practice Admin and users with the 'Biller' role can access the RCM dashboard. It contains various detailed reports of claims and their payments.
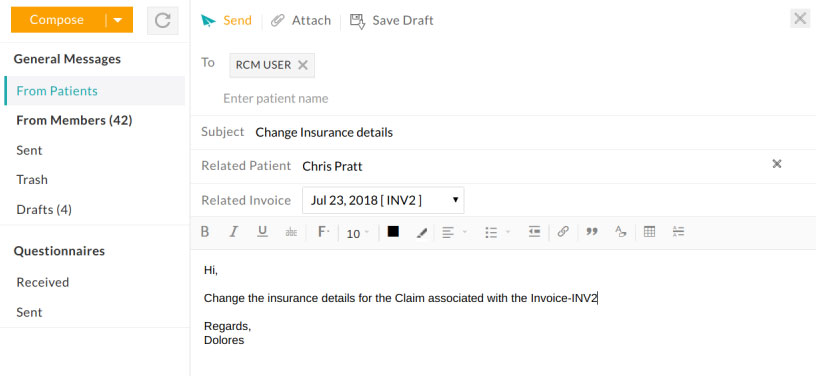
The messages section helps in the exchange of information between practice and RCM in a secure way. Messages to RCM can be sent by selecting the RCM USER in the 'To address' field. Refer to the screenshot below. Attachments can also be sent along with messages. Practices/Providers can send messages either from their EHR 'Messages' section or from RCM Dashboard 'Messages' section. Messages sent from RCM to the provider will be available in the 'From Members' folder of the messages section.
Post RCM Submission actions
Applying Explanation Of Benefits (EOB) - by RCM
In general, the payer will process the claim and send EOB in 1 to 4 weeks after claim submission. The RCM team has access to any EOB that comes to practice's Optum account. For the EOBs not coming to Optum, practice will receive a copy of EOB from Payer. These EOBs should be sent to the RCM team using 'Messages', which is a secure messaging system.
As part of RCM service, details available in EOB, such as
- Insurance Payment
- Contractual Adjustment (Contractual Obligation)
- Patient Responsibility (PR), which includes copay, coinsurance, deductible, not covered charges will be posted against the claim. Insurance payments, Contractual Adjustments, PR will be added to the invoice automatically. This workflow is explained below with a sample EOB.

In the above EOB, the first CPT-99214 has
- An Insurance payment of $92.32
- Adjustment of $49.68
- Patient Responsibility (copay) of $20.00.
- Similarly, second CPT has payment of $16.33 and Adjustment of $9.67,
- Third CPT has payment of $14.94 and adjustment $13.06.
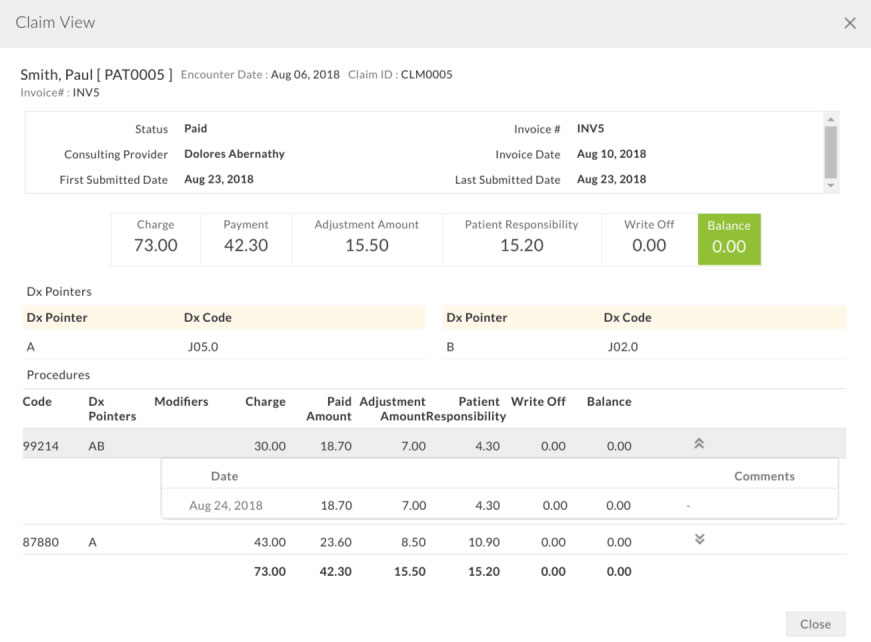
These payments, adjustments and patient responsibilities will be added to each line item of the claim. Total payment and total adjustments will be added to the invoice and invoice due will be reduced accordingly. Patient Responsibility will be shown as a note in the invoice.
- Total payment - $123.59
- Total contractual adjustment - $72.41
- Total patient responsibility - $20.00
can be seen in the Invoice summary.
As patient copay was not collected at the time of visit, the invoice due of $20.00 can be seen, which is patient responsibility. The same invoice can be sent to the patient for the payment of patient responsibility. This is how payments, adjustments, PR in EOB will reflect in the Invoice (created for the patient visit) in EHR.
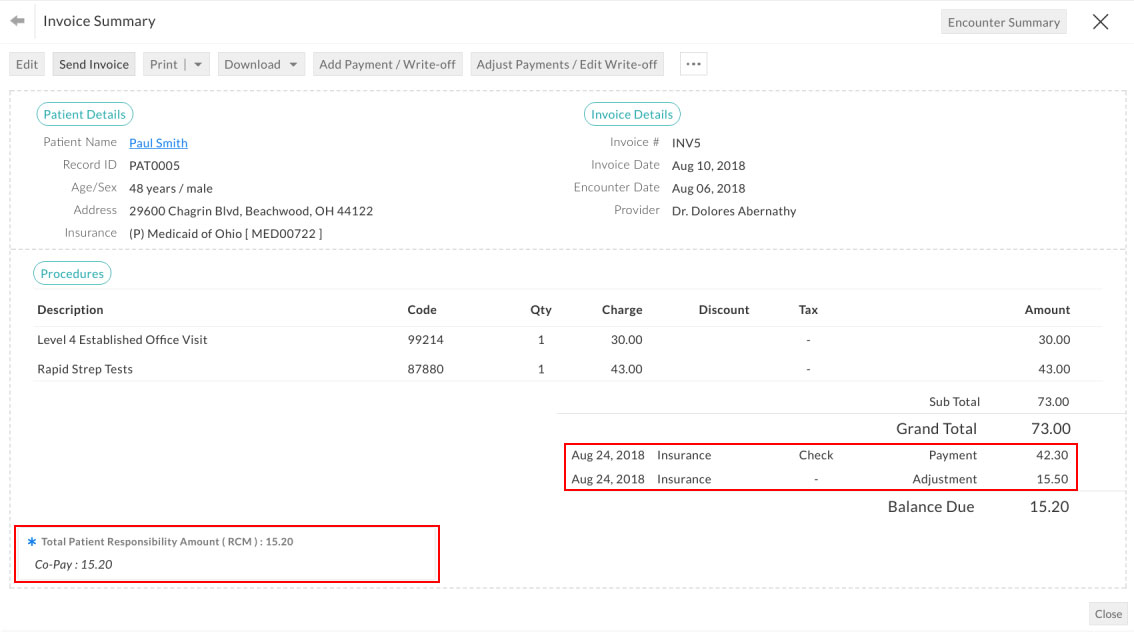
Practice can check CPT level payments, adjustments and patient responsibilities by clicking the 'Claim View' option available for RCM submitted Invoices. Refer to the screenshots below.
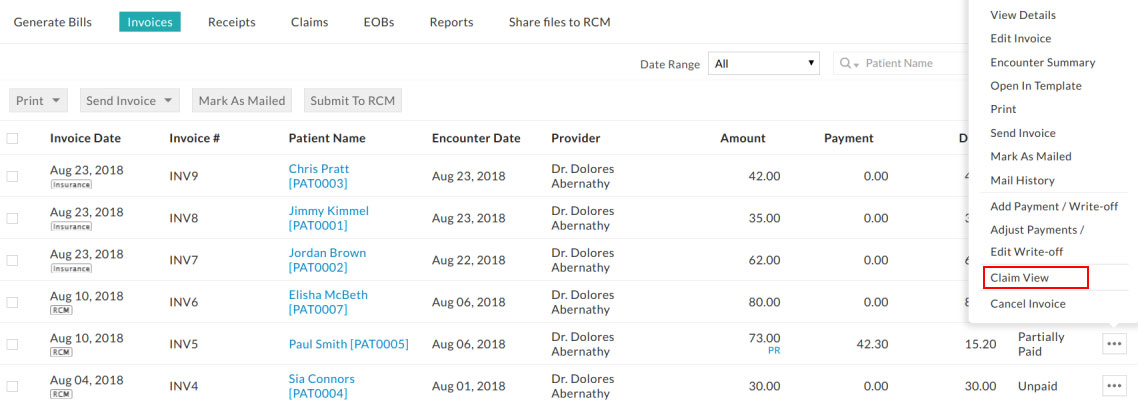
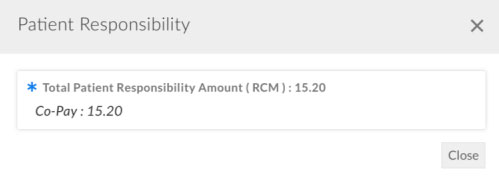
Managing Invoices with Patient Responsibility
All the invoices with patient responsibility are marked with PR or PR-SEC.EXISTS (this means that Invoice has PR and the patient has secondary insurance to process secondary claim) link in the invoice list view. Detailed PR information, copay, coinsurance or deductible will be shown on clicking these links. Refer to the screenshot below.
Invoices with PR can be better managed with 'RCM Claim Options' available in the EHR Invoices section.
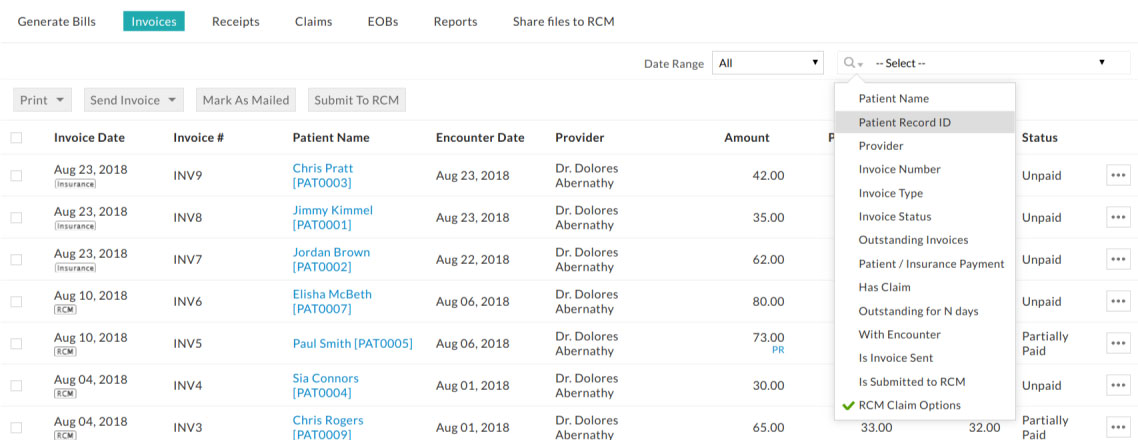
'RCM Claim Options' has following filter options
| Claim Status | Description |
|---|---|
| Has PR | Lists invoices having patient responsibility |
| Has No PR | Lists invoices having no patient responsibility |
| Has PR - Secondary Exists | Lists invoices having patient responsibility and patients having secondary insurance. i.e. Secondary claim can be processed for these patients. |
| Has PR & Invoice Due | Lists invoices with due and having patient responsibility. When patients pay for the PR dues, invoices will not be listed here. |
| Has PR, Due & Not sent to patient | Lists invoices with due, having patient responsibility and it is not mailed, emailed or sent to patient portal (PHR). |
Practices having invoices in 'Has PR & Invoice Due' means that invoices are awaiting patient payment. Few invoices in this view mean that Account Receivable (AR) from the patient is low.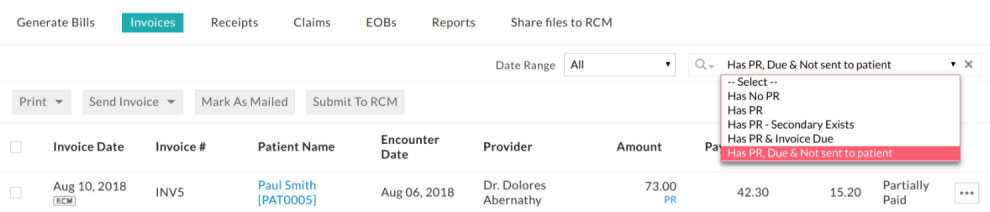
RCM Dashboard for Practice Members
'Claim Report' available in RCM Dashboard (login to https://rcm.charmtracker.com) lists all the claims Generated at RCM along with the claim status. When a claim is paid, it shows payments, adjustments, and patient responsibility. Refer to the screenshot below.
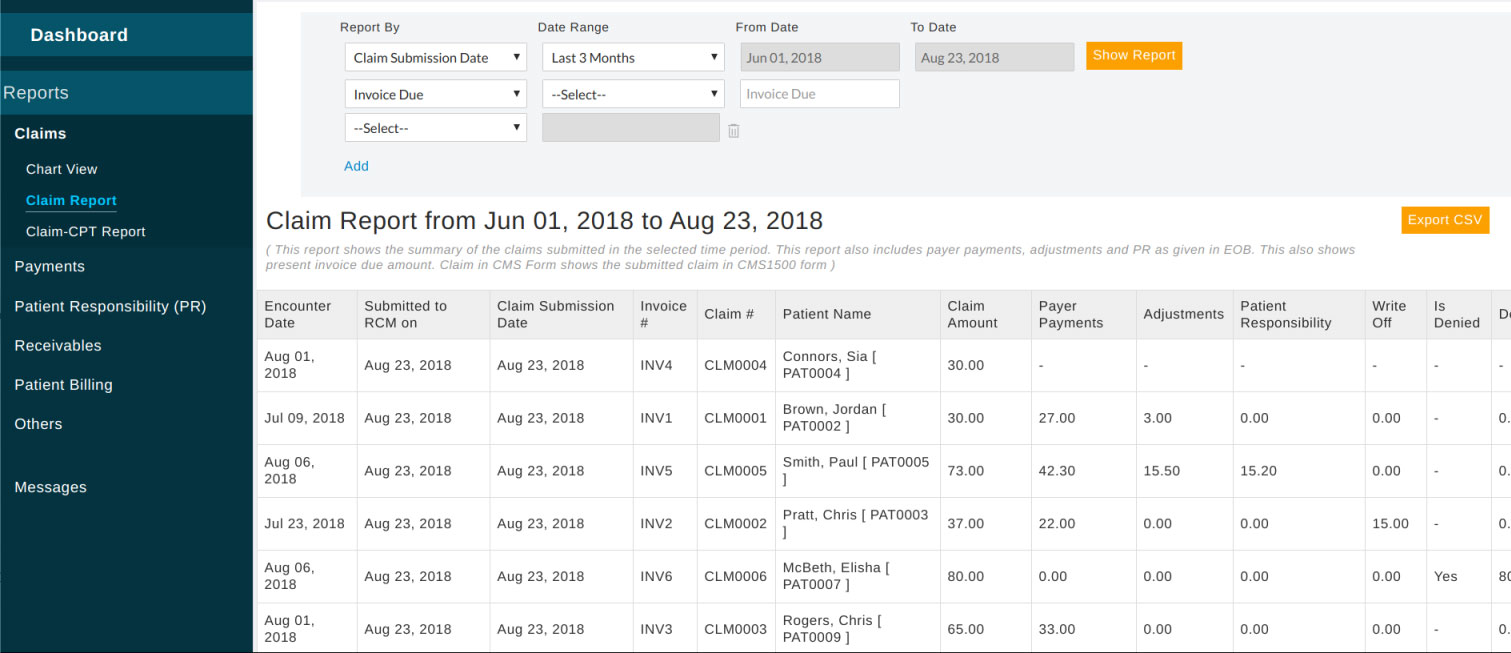
Claim status and its description:
| Claim Status | Description |
|---|---|
| Submitted | Claim submitted to clearing house |
| Resubmitted | Claim resubmitted to the clearing house, either after Rejection or after denial |
| Reprocessing | Payer agreed to reprocess the claim |
| Denial | Claim has been denied by Payer |
| Paid | Claim has been paid by the insurance company. It may have adjustments and patient responsibilities |
| PartiallyPaid | Received payment from insurance company. Claim still has some due |
| Closed-PR | Closed claim with no payment. It has patient responsibility. May have adjustments |
| Closed-Adjustment | Closed claim with complete claim charge as Contractual Adjustment |
| UnPaid | Claim with no payment. May have patient responsibility or adjustment. Claim still has due. |