Electronic Claim Submission
All the claims generated will be listed in the 'Billing > Claims' section. The claims can be electronically submitted from CharmHealth to the payers with a click of a button, without logging into the Clearinghouse account. Upon successful submission, the status of the Claims will be automatically changed to 'Submitted Electronically'. One can select multiple claims and submit them to payers. The process of Claim generation and submission is explained in this section.
Generating Claim from Invoice
To generate a claim for an invoice, go to the 'Billing > Invoices' section. Select the 'More Options' (...) icon against the invoice and click on the 'Generate Claim (CMS1500)' option.

Generating Claims for Multiple Invoices
If you need to generate the claims for multiple invoices, then select the invoices and click on the 'Generate Claims' button.

Once the claims are generated, a preview of the claims is shown. If there are any warnings/errors, it is indicated by a warning sign beside the claim. You can navigate to the claim and edit as required.

Automatic Claim Generation
CharmHealth has a feature to generate claims automatically as and when an invoice for an encounter gets approved. This saves the user time in generating the claims manually. The user can configure the necessary settings for claim generation as explained in the 'Claim Generation Settings' section.

Edit Claim
To make any corrections to a claim, click on the 'Edit Claim (CMS1500)' option under the 'More Options' (...) icon against the claim.

Claim Generation Settings
The Claim Generation settings provide various options to make the claim generation simpler and faster by configuring the default values.
Go to the 'Billing-Claims > Claim Settings' section to configure the settings.

The options are briefly explained below as shown in the screenshot.

(1) Diagnosis Re-ordering - Choosing the option 'Yes' enables Dx codes re-ordering in both Invoice and Claim.
(2) Add/Delete Diagnosis - This option controls the addition and deletion of Dx codes from the claims.

(3) Secondary Claim Processing - To configure whether the Practice prefers to process the secondary claims before billing the Patient. This affects various reports, Patients, and insurance balances as well.
(4) Automatic Claim Generation - Select 'Yes' to enable automatic claim generation when an invoice for an encounter gets approved.
(5) Claim Primary Insurance selection - To configure which insurance should be selected as the Primary insurance in a claim
(6) Claim Secondary Insurance selection - To configure which insurance should be selected as the Secondary insurance in a claim
(7) Rendering Provider - Choose which Provider has to be populated as the Signature Provider(box #31)
(8) Procedures - Choose whether to add all the procedures from the invoice (or) exclude the non-covered services.
(9) Billing Provider - You can select either one Billing Provider to populate all the claims generated across the Practice, or else choose a specific Billing Provider for each Facility.

(10) Service Facility - Decide whether to select the Facility of the encounter (or) choose any one Facility always.
(11) Prior Authorization/CLIA # Preference - When both Prior Auth # and CLIA # are configured, which one is preferred to populate in the claim.
(12) Prior Auth # Selection - Option allows the system to decide one prior auth # out of the multiple prio auth #'s added to a Patient's insurance.
(13) Referring Provider - Set up whether to choose the Patient's Referring Provider (or) any specific Provider in all claims generated across the Practice.
(14) Release medical information - Decides whether to take the value from the respective Patient's insurance (or) a specific value(Yes/No) in all the claims.
(15) Assign medical benefits - Select whether to read this value from the Patient's insurance (or) any other default value from the list.
(16) Accept Assignment - Select the default value to be populated in all claims to indicate whether the Provider accepts the benefits under the terms of the payer’s program.
(17) Amount Paid - Choose to fill in the payment added to the invoice (or) leave blank.
(18) E-claim Submitter Type - Choose whether to select an individual consulting Provider (or) the claim Facility as the default submitter.
(19) Pay-to Address - Choose the default Pay-to Address to be populated in all the claims across the practice (or) set up one Pay-to Address for each Facility.
Submitting Claims Electronically
On clicking the 'e-Claim Submission' button under the 'Billing > Claims' section, the Claims that are ready for submission get listed.

Multiple Claims can be selected and submitted from the list by clicking on the 'Submit To Payers' option. On submitting the Claims, CharmHealth validates the Claim details and prompts for any missing or invalid information in the Claim. The Data Validation section in this document explains more about the validation.
Claim Submission Options
i) For Optum Clearinghouse
Users integrated with OPTUM Clearinghouse can submit the claims using the 'Submit To Payers' option.

- The claims will get submitted to Optum in the back end, and the response will be shown in the view. You can also move away from the eClaim submission view and check the results later by accessing the 'eClaim Submission History' section anytime later.
- The Claim submission response shows a summary of the claims Accepted and Rejected.
- The 'Claim submission is successful' message indicates that the claim has been transmitted to the Clearinghouse successfully, and the claim status gets updated to 'Submitted Electronically'.
- The Clearinghouse will submit these Claims to the Payers periodically.

ii) For Change Healthcare Clearinghouse
e-Claim Submission Option for Change Healthcare Clearinghouse

Submit to Payers
- When you submit the claims using the 'Submit to Payer' option, the claims get scheduled for submission, and the status changes to 'Scheduled for Submission'.
- Once the claims get transmitted to Change Healthcare, the status gets updated to 'Submitted Electronically'.
iii) Download Claim ANSI 837P Files (For the Payer with no support for Electronic Claim Submission)
For Practices submitting the Claims to the Payers not supported by your Clearinghouses (Optum or Change Healthcare), Charm offers the ability to download the Claims in ANSI 5010 (837P) format. You can upload them to the Payer portal.
To download the ANSI files, follow the steps given below.
- Navigate to 'Billing > Claims > e-Claim Submission'. The Claims that are ready for submission to the Payers with the statuses 'Not Submitted' and 'Ready for re-submission' are listed.
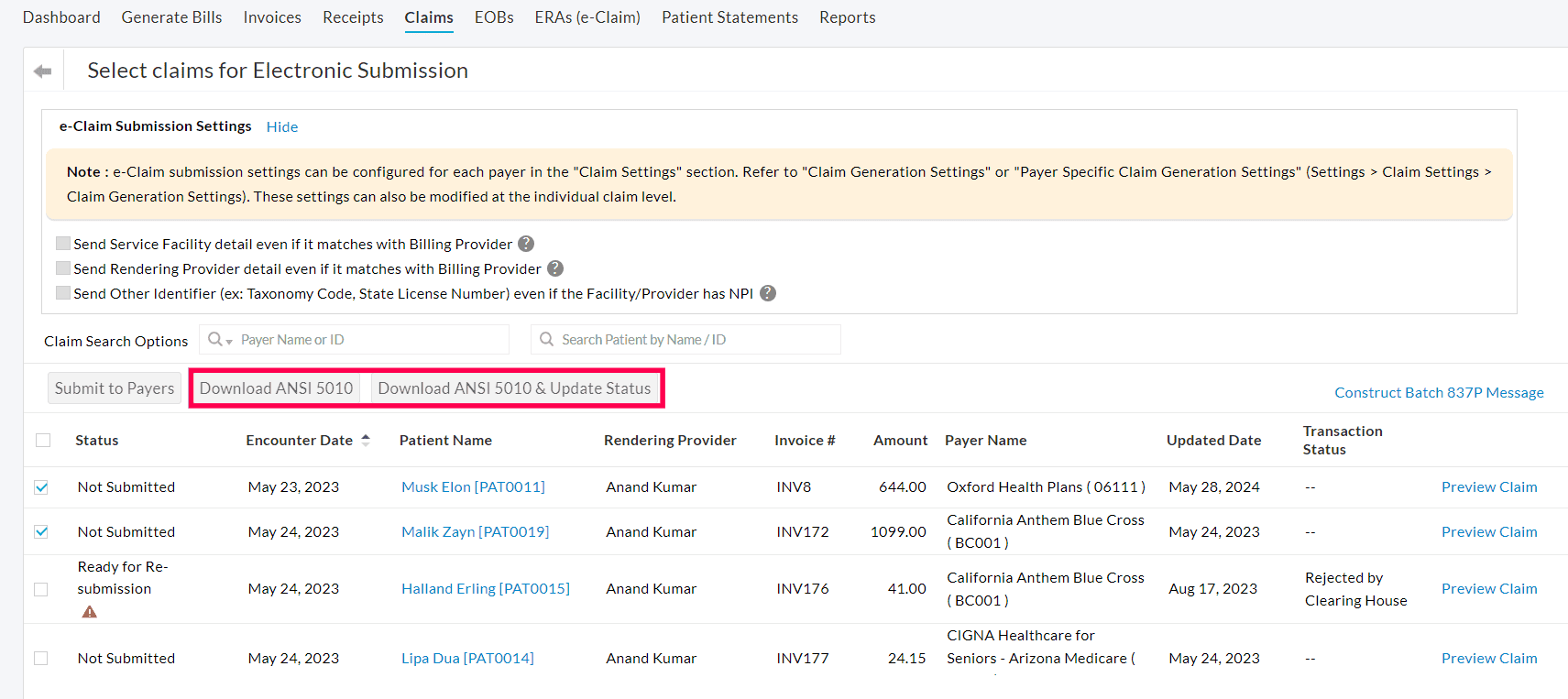
- Select the required Claims and click the 'Download ANSI 5010' button to download the ANSI 5010 file for the selected Claims.
- If you need to download the ANSI Files and update the status of the Claims to 'Submitted' or 'Re-submitted', use the 'Download ANSI 5010 & Update Status' option.
Data Validation Before Claim Submission
A submitted claim will get rejected if it has missing data or contains invalid data as per the ANSI 5010 specification. To avoid this, CharmHealth validates the claim information before submitting them to the Clearinghouse. The claims having any missing/invalid data will not be submitted to the Clearinghouse, and the relevant errors will be shown. Other claims without any issues will be sent to the Clearinghouse.
CharmHealth validates the following information.
- Submitter (consulting Provider/Service Facility) details
- Billing Provider Details
- Subscriber Details
- Payer Details
- Patient Details
- Other Claim Details

Below is the list of possible error messages with a brief description of each error. A procedure for correcting these errors is also given.
Claim Submitter Detail is mandatory. Select the Submitter.
The Submitter is either the Provider of the Practice or Facility. By default, the consulting Provider of the Encounter gets selected as the Submitter. Edit the claim using the 'Edit Claim(CMS 1500 Form)' option and scroll to the bottom of the view to the 'eClaim Additional Details > Submitter Details' section. Choose the appropriate submitter below the Box#31.
The contact information of the Submitter is required. Provide at least one of the contact details given below.
- Phone Number
- Fax
The Submitter contact detail is mandatory as per the ANSI 5010 specification. If the Submitter is a Provider, go to the 'Settings > Facility > Facility Members' section, edit the respective Provider, and provide the Phone Number, Fax, or Email of the Provider. If the Submitter is a Facility, go to the 'Settings > Facility > Facility List' section, edit the Facility, and update the contact information. Then, you can edit the claim, re-select the submitter in the bottom of the claim CMS 1500 Form wizard under the 'eClaim Additional Details -> Submitter Details' section, and save the claim.
Enter 9 digit ZIP code for Billing Provider
The ZIP code must be 9 digits (i.e, 5 digit ZIP and 4 digit Postal Code) for Billing Provider and Service Facility. Go to the 'Settings > Billing-Claims > Billing Provider' section, edit the 'Billing Provider', and update the ZIP and Postal code. Then, edit the Claim, scroll to box#33. 'BILLING Provider INFO & PH #' in the CMS 1500 Form claim wizard, click on the Refresh (  ) icon adjacent to the Provider name drop-down, and save the Claim.
) icon adjacent to the Provider name drop-down, and save the Claim.
A Billing Provider Identifier is required. Enter any of the following identifiers.
- NPI
- State License Number (0B)
- Provider UPIN Number (1G)
The Provider Identifier is mandatory for the Billing Provider. You can edit this 'Billing Provider' under the 'Settings > Billing-Claims > Billing Provider' section and update it with NPI. Then, edit the claim, scroll to box#33. 'BILLING Provider INFO & PH #' in the CMS 1500 Form claim wizard, click on the Refresh (  ) icon adjacent to the Provider name drop-down, and save the claim.
) icon adjacent to the Provider name drop-down, and save the claim.
A rendering Provider Identifier is required. Enter any of the following Identifiers
- NPI
- State License Number (0B)
- Provider UPIN Number (1G)
- Provider Commercial Number (G2)
- Location Number (LU)
The Rendering Provider Identifier is mandatory. You can edit the Provider under the 'Settings > Facility > Facility Members' section and update the NPI. Then, edit the claim, scroll to box#31. SIGNATURE OF PHYSICIAN OR SUPPLIER INCLUDING DEGREES OR CREDENTIALS' in the CMS 1500 Form claim wizard, click on the Refresh (  ) icon adjacent to the Provider name drop-down, and save the claim.
) icon adjacent to the Provider name drop-down, and save the claim.
Enter 9 digit ZIP code for Service Facility
The Service Facility must have a 9 digit ZIP code (i.e, 5 digit ZIP and 4 digit Postal Code) for Electronic claim submission. Edit the Facility under the 'Settings > Facility > Facility List' section and update it with the ZIP and postal code. Then, edit the claim, scroll to box#32. 'SERVICE FACILITY LOCATION INFORMATION' in the CMS 1500 Form claim wizard, click on the Refresh (  ) icon adjacent to the Facility name drop-down, and save the claim.
) icon adjacent to the Facility name drop-down, and save the claim.
A service Facility Identifier is required. Enter any of the following Identifiers
- NPI
- State License Number (0B)
- Provider Commercial Number (G2)
- Location Number (LU)
An Identifier is mandatory for the Service Facility. Go to the 'Settings > Facility > Facility List' section and update it with the Facility NPI. Then, edit the claim, scroll to box#32. 'SERVICE FACILITY LOCATION INFORMATION' in the CMS 1500 Form claim wizard, click on the Refresh (  ) icon adjacent to the Facility name drop-down, and save the claim.
) icon adjacent to the Facility name drop-down, and save the claim.
Select the 'Policy Type Code' for Secondary Insurance [MEDICARE]
As per the ANSI 5010 specification, 'Policy Type Code' is mandatory when MEDICARE is the 'Secondary Insurance' in the Claim. Edit the claim, scroll to the 'eClaim Additional Details > Other Details > Policy Type Code' section, choose the appropriate value, and save the claim.
Diagnosis codes related to this service (24.E) are not specified. Select the Related Diagnosis Codes
This is shown when Dx codes are not mapped to a CPT. To correct this, edit the Claim and the respective CPT by clicking on the 'Edit' icon against the CPT, map the Dx codes, and save the claim.
eClaim Submission History
- Click on the 'e-Claim Submission History' button in the 'Billing > Claims' section to view the past transactions of the submitted claims. The response details can be viewed by clicking on the 'View' option.


- The 'Submission response' can also be viewed by clicking on the 'e-Claim Transactions' option against the claim as shown below.

Handling Rejections in CharmHealth and Re-submitting a claim
Sometimes, the Payers will reject the Claim if there is some issue with the claim details like the Patient's insurance ID. The best practice would be periodically checking and tracking the 'Transaction Status' of the claims.

Many payers provide some level of a report about the submitted claims, such as 'Acknowledged by Payer' or 'Accepted by Payer' or 'Rejected by Payer'. However, there are a few payers who do not provide the claim reports. As a best practice, the biller has to periodically check for claims still in submitted status without any rejection and EOB, and then call the payer to know the status.
Clicking on the rejection status, for example, 'Rejected by Payer', will give more details about the rejection. The user has to check the respective rejection reason, make the required corrections to the claim, and resubmit the Claim.

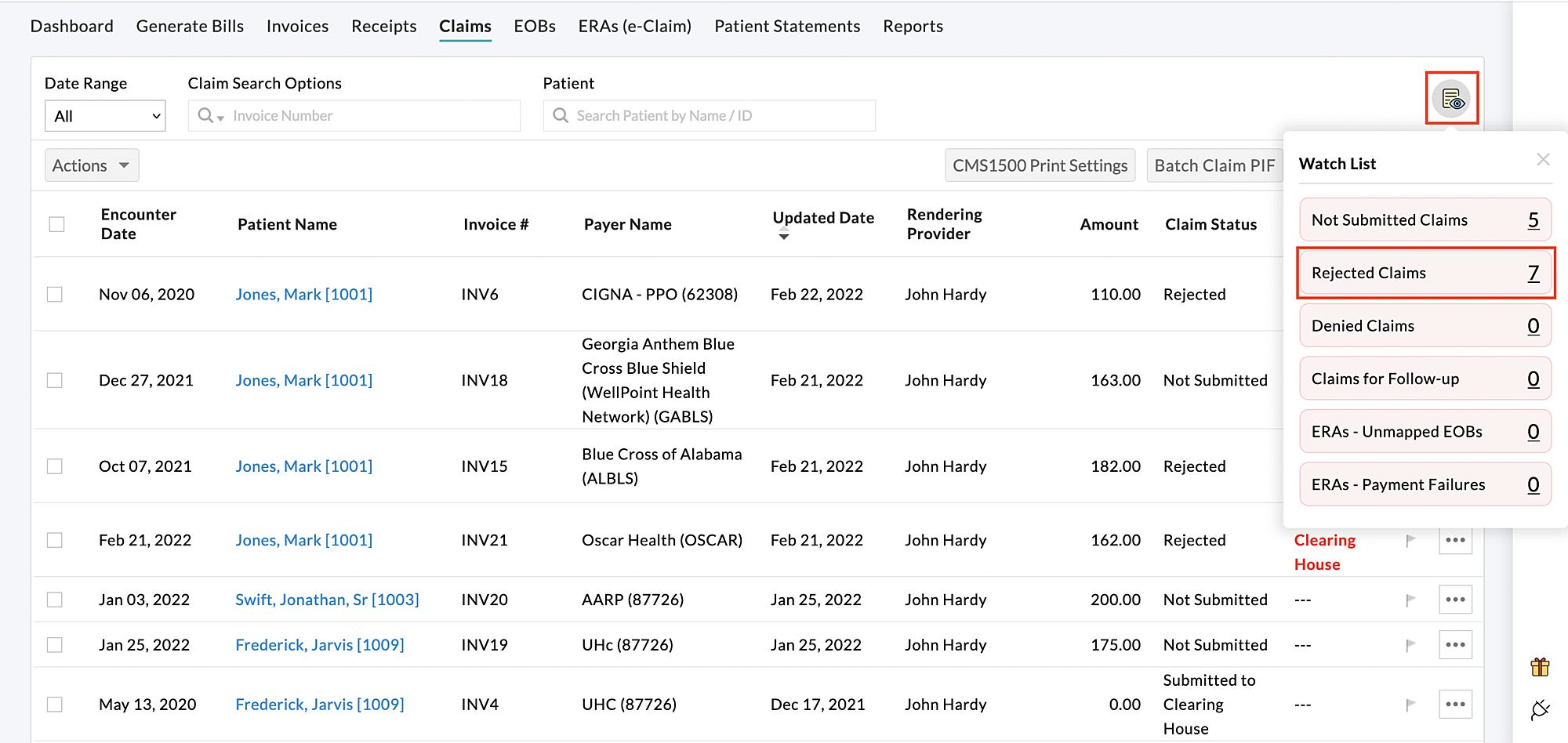
You can also use the 'Watchlist' option to view any rejected Claims quickly.
Configure Role-Based Access to e-Claim Submission
Access to ERA and e-Claim submission are given to the Practice Admin and Biller roles by default. These permissions can also be given to other users using Role-Based Access in EHR.
e-Claim Permissions
Enable the 'Export (PDF to print on CMS1500 form, PIF for Optum)' option for any role to allow the members in that role to submit the claims electronically.
