Supported Clearinghouses
Optum Supported Payer List
Visit the Optum Payers List page and go to the 'Optum Revenue Cycle Payer Lists' section to access the supported payers list for Real-time Eligibility, Electronic Claim Submission, and Electronic Remittance Advice (ERA) transactions.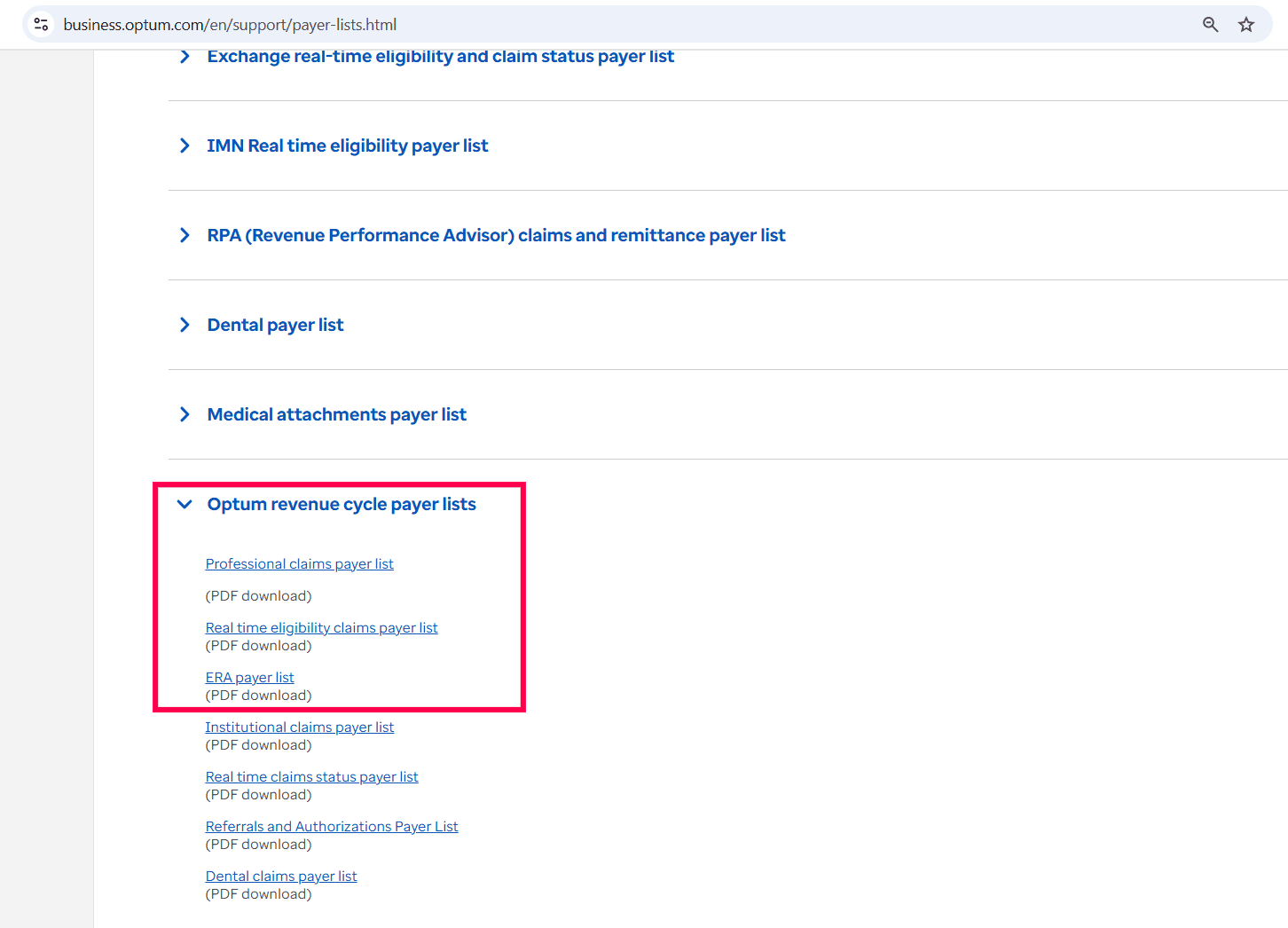
Access the direct URL for:
Real-time Eligibility - https://customerconnect.optum.com/payerlist/IediRealTime
Electronic Claim Submission (Claims - Professional, 837P) and Electronic Remittance Advice download (ERA, 835P) - https://customerconnect.optum.com/payerlist/IediClaimsAndEra
Enrollments for Optum
Practice needs to do ERA enrollment with the Payers to get the ERAs to the Clearinghouse account automatically. A few Payers require enrollment to use Eligibility and for Electronic Claim Submission.
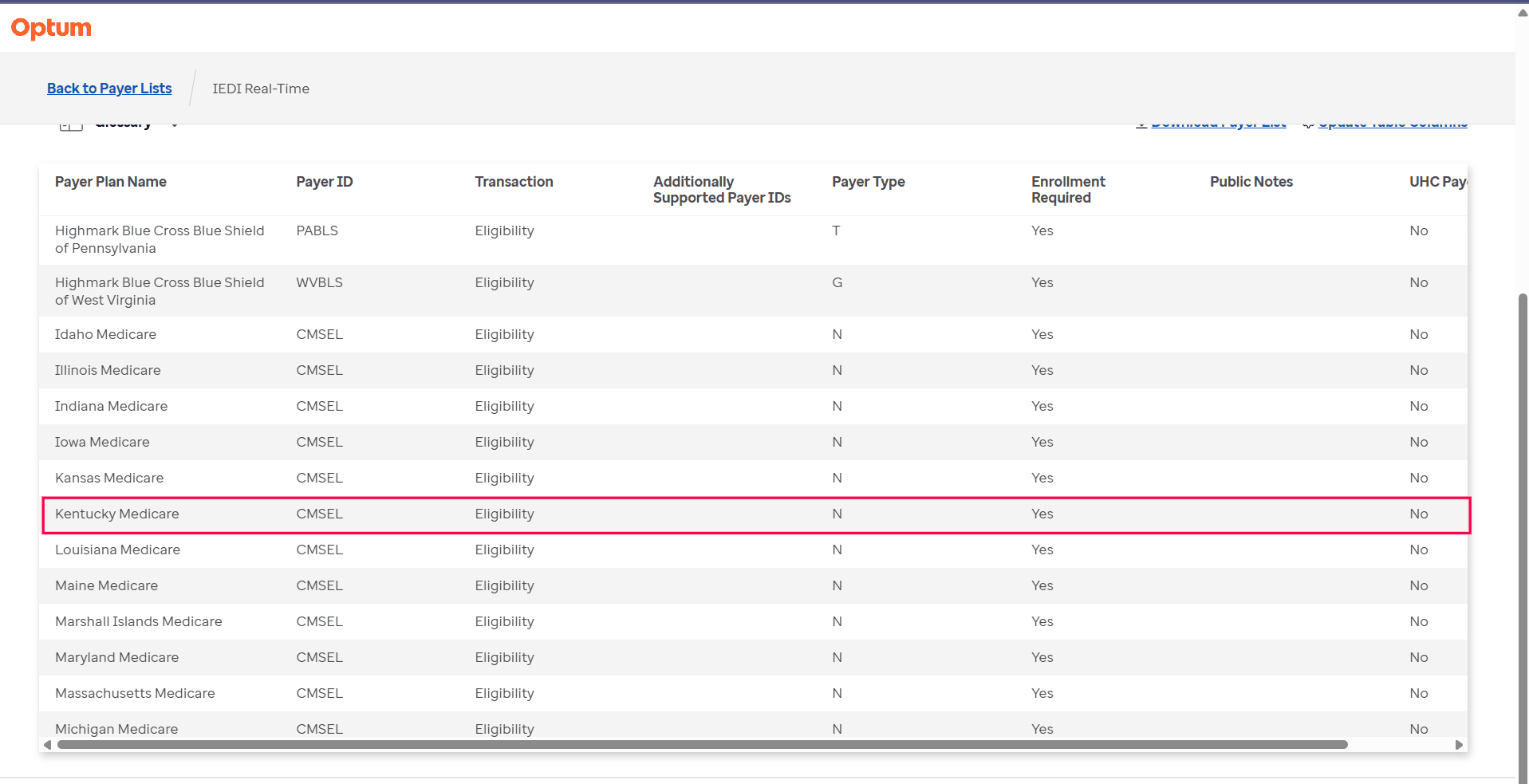
(i) Eligibility Enquiry:
A few Payers that need enrollment to do eligibility checks are:
- Medicare and Medicaid plans
- Some commercial payers such as Kaiser Permanente Northern CA and Michigan Blue Cross Blue Shield
To view the complete list of Payers that need enrollment for Eligibility Checks, go to the IEDI Real-Time page. Filter the Transaction type by 'Eligibility' and set 'Enrollment Required' to 'Yes' to display all applicable Payers.
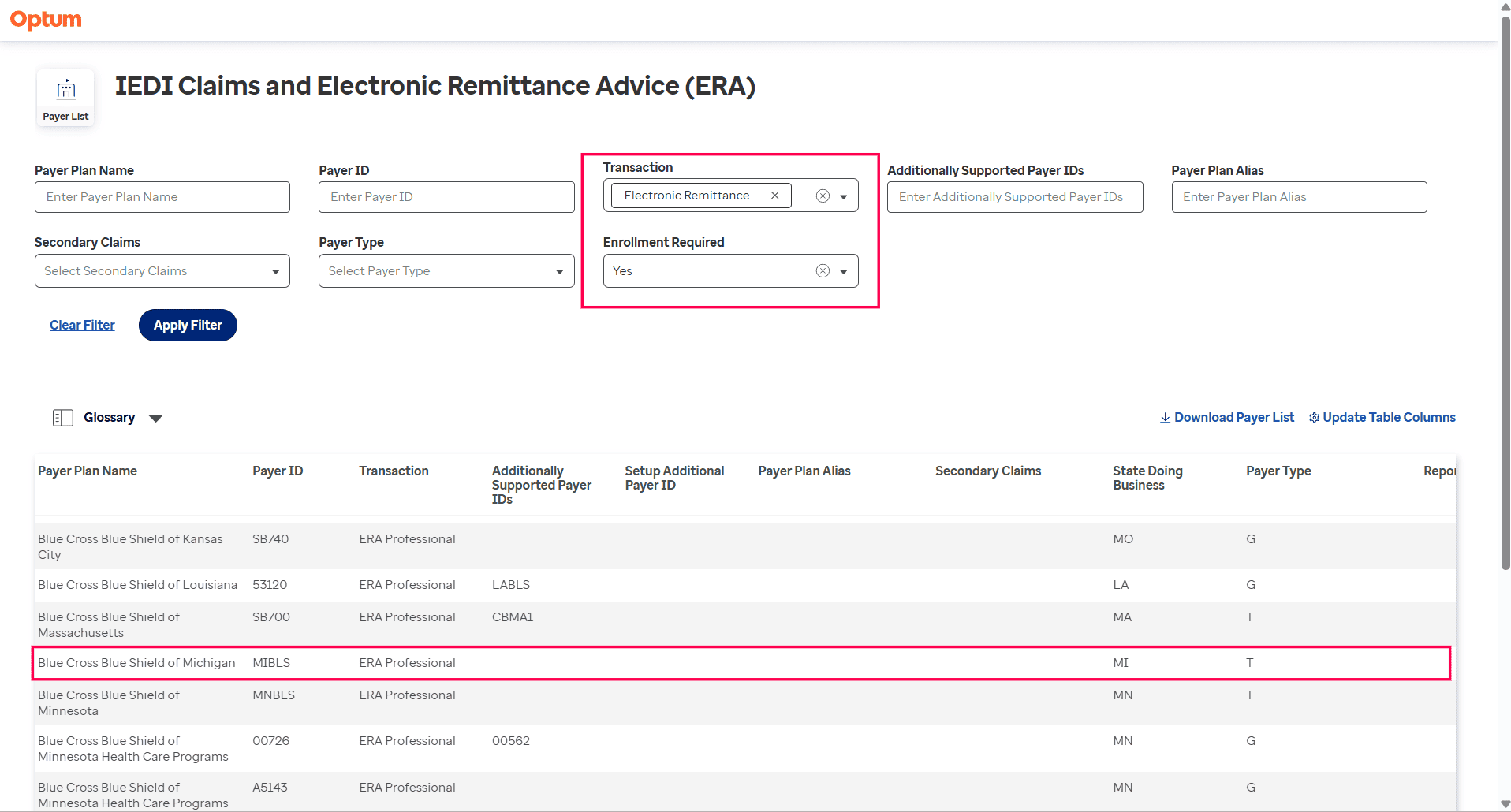
(ii)Electronic Claim Submission
A few payers that need enrollment for Electronic Claim Submission are:
- All Medicare and Medicaid plans
- Majority of Blue Cross/Shield plans
- Avalon Healthcare Solutions North Carolina
- Beacon Health Strategies
To view all Payers that require enrollment for Electronic Claim Submission and ERA, go to the 'IEDI Claims and Electronic Remittance Advice (ERA)' page and select 'Claims - Professional' or 'Electronic Remittance - Professional' for the 'Transaction' filter and set 'Yes' for 'Enrollment Required'.
For Any other Clearinghouses
Charm offers an ANSI package for Practices that use any other Clearinghouses besides Optum, such as the following.
- Download Claim ANSI 837P Files: This option allows the Practices to download the Claims in ANSI format and upload them to the desired Clearinghouses.
- Upload ERA ANSI 835 Files: Practices can get the ERA 835 Files from the Payer portal and upload the same in Charmhealth.
To enable the above options, Charm requires specific details from the Practice's Clearinghouse for ANSI 837, as given in the table below.
| Segment Name | Loop/Segment/Element | Value (?) | Comments |
|---|---|---|---|
| INTERCHANGE_SENDER_ID | ISA06 | An alphanumeric value. The maximum length is 15 characters. Provided by Clearinghouse. For example, Practice's TIN |
|
| INTERCHANGE_RECEIVER_ID _QUALIFIER | ISA07 | Allowed values are, 01, 14, 20, 27, 28, 29, 30, 33, ZZ Example Value - ZZ |
|
| INTERCHANGE_RECEIVER_ID | ISA08 | An alphanumeric value. The maximum length is 15 characters. Provided by Clearinghouse. For example, Clearinghouse (or) third-party TIN to whom you will upload the ANSI Claim file. |
|
| APPLICATION_SENDER_CODE | GS02 | An alphanumeric value. The maximum length is 15 characters. Provided by Clearinghouse. For example, Practice's TIN |
|
| APPLICATION_RECEIVER_CODE | GS03 | An alphanumeric value. The maximum length is 15 characters. Provided by Clearinghouse. For example, Clearinghouse (or) third-party TIN to whom you will upload the ANSI Claim file |
|
| SUBMITTER_NAME | Loop 1000A NM103 NM104 NM105 |
Charm allows either consulting provider of the Claim or Service Facility. Let us know which has to be sent here. |
|
| SUBMITTER_ID | Loop 1000A NM109 |
An alphanumeric value. The maximum length is 15 characters. Provided by Clearinghouse. For example, Practice's TIN |
|
| RECEIVER_NAME | Loop 1000B NM103 |
Sixty-character length alphanumeric value. For example, the Name of the Clearinghouse/ |
|
| RECEIVER_ID | Loop 1000B NM109 |
An alphanumeric value. The maximum length is 15 characters. Provided by Clearinghouse. For example, the Clearinghouse (or) third-party TIN to whom you will upload the ANSI claim file. |
For more details, contact our dedicated support team at support@charmhealth.com.