Real-time Eligibility Inquiry
CharmHealth uses the Clearinghouse service to get the Patient's insurance eligibility information from the Payer in real time.
Check Insurance Eligibility
From Patient Dashboard
- For the Practices enabled with this feature, the 'Check Eligibility' option will be enabled under the 'More Options' (...) icon in the Patient's Dashboard.

- Clicking on this option navigates the user to the 'Insurance Eligibility' view.
- Select the Patient's insurance, Provider, Service Type, and Date of Service to complete the eligibility check.

- Add Insurance & Edit Insurance - Options to Add new Insurance and Edit the selected Insurance are provided on this page.
- Insurance - All the Insurances added for this Patient get listed in the Insurance drop-down. The Payer name is shown along with the 'Eligibility Supported' or 'Eligibility Not Supported' text. This additional text indicates whether the eligibility check is supported for this Payer or not.
- Provider- The Providers list shows all the Providers and Facilities in the Practice. Refer to the 'Insurance Eligibility Settings' section to learn more about configuring the default Service Provider.

- Service Type - The Service Type field lists all the service types supported by the Payer. Refer to the 'Insurance Eligibility Settings' section to learn more about configuring the default ServiceType.

- The Patient details on the right-hand side will be sent with the eligibility request. Using these details, the Payer will search their database for the Patient's Insurance. Some Payers need additional details of the Patient such as SSN, Medicare ID, etc.
- Click on the 'Check Eligibility' button after selecting the appropriate details. CharmHealth sends an eligibility request to the Payer via your subscribed Clearinghouse and renders the response in a readable format. The eligibility information is separated based on the service type code in the response received. Select the service type code to view the eligibility details for the specific service type.

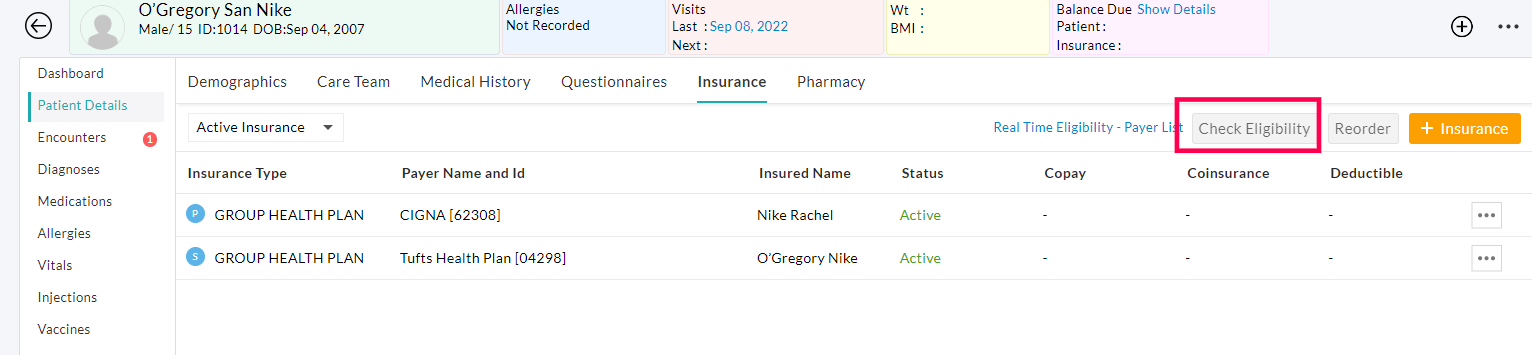
From Patient Dashboard - Insurance section
The 'Insurance Eligibility' option is provided in the Patient's insurance section as well. Refer to the below screenshot.

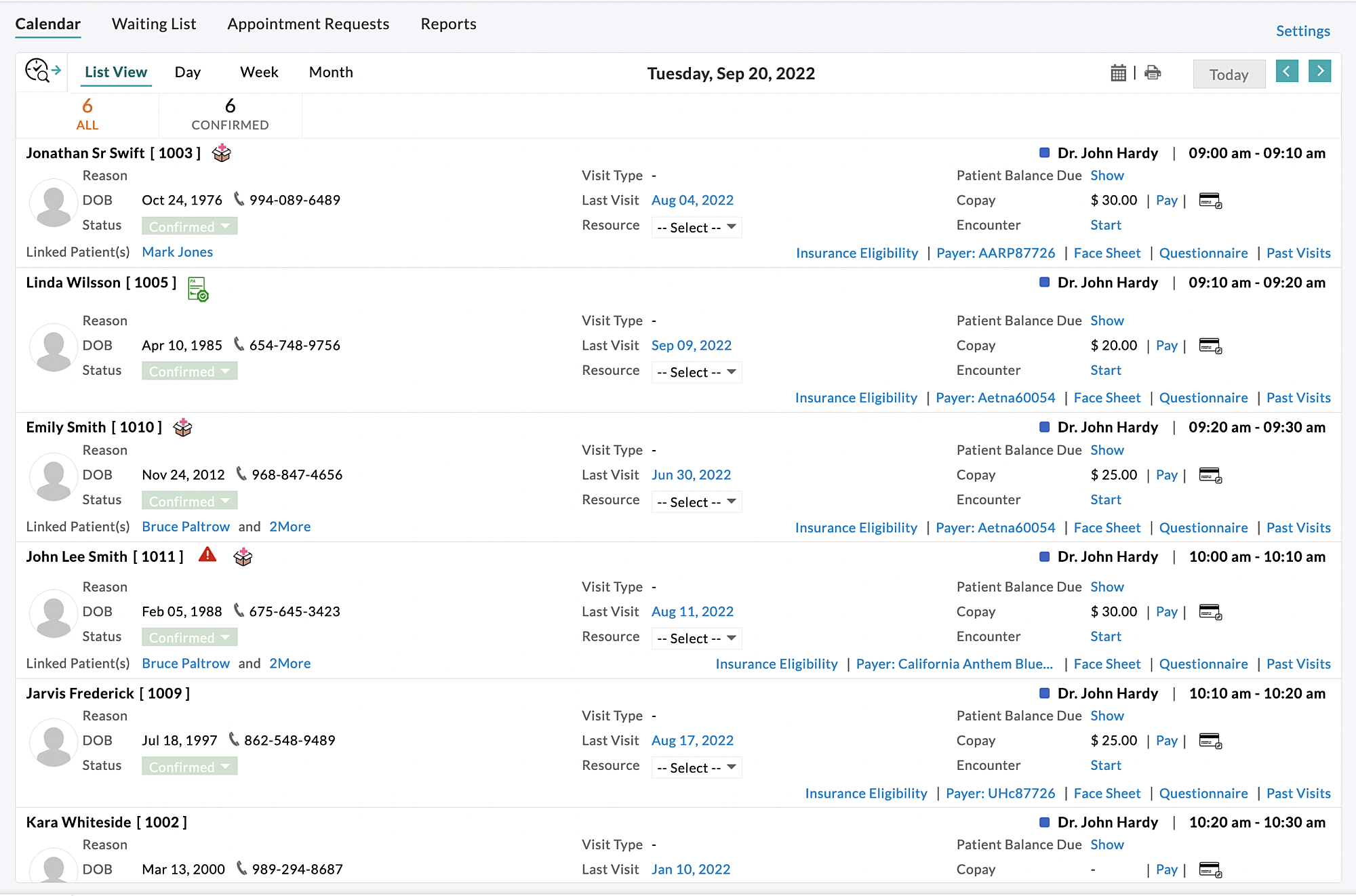
From Calendar - Appointment List View
The 'Insurance Eligibility' option is also provided in the Appointment list view for easy verification of the eligibility details by the Front office.
Insurance Eligibility History of a Patient
- The eligibility benefit information is stored and can be accessed in the future. To access the past eligibility details, click on the 'Eligibility History' option.

- All the past eligibility benefit details get listed in chronological order. Selecting any past eligibility request from the list will show the respective eligibility details.

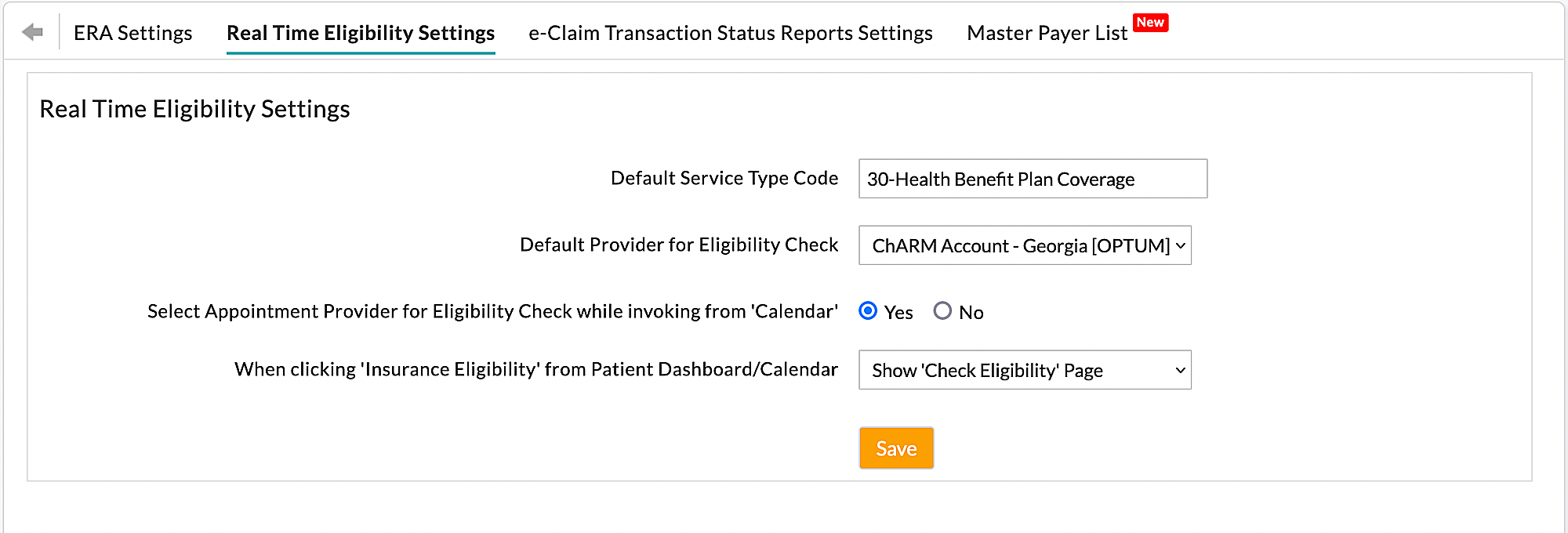
Insurance Eligibility Settings
Practice can set the preferred 'Service Type Code' and 'Provider' for the eligibility verification from the 'Settings > Billing-eClaims > Real Time Eligibility Settings' section under the following fields, 'Default Service Type Code' and 'Default Provider for Eligibility Check'.
Also, the Practice can configure the Provider to be chosen in the eligibility view that gets invoked from the 'Calendar' section.
Adding/Updating Eligibility Payer ID of the Patient's insurance
The list of Payers supporting real-time eligibility requests is available under the 'Settings > Billing-eClaims > Master Payer List' section. The Payers can be searched with the Payer Name or Payer ID, Eligibility Payer ID, or ERA Payer ID. If a Payer has a separate Payer ID for eligibility under the 'Eligibility Payer ID' column, then the same has to be entered under the 'Eligibility Payer ID' field while adding the Payer.
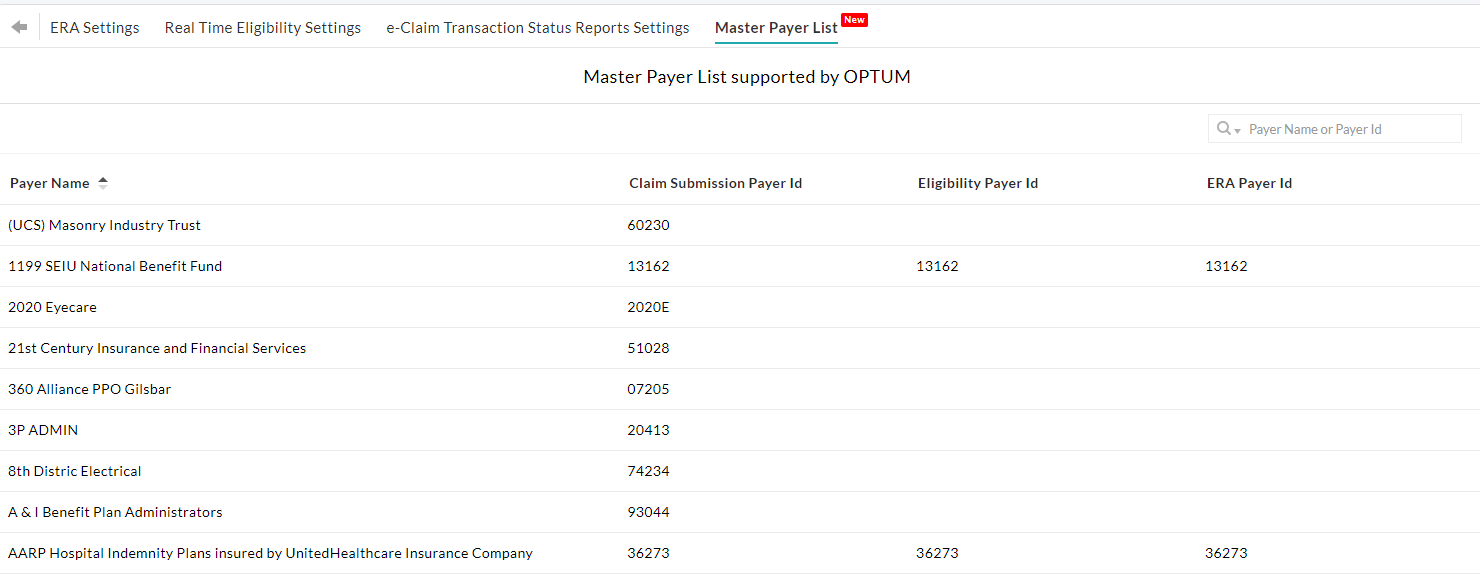
All payers added in the Practice are listed under the 'Settings > Billing - Claims > Payers'. In order to add/update the Eligibility Payer ID, click on the 'More Options' (...) icon against the payer, select the 'Edit' option,and update the Eligibility Payer ID.

Typical Error Messages
- Missing mandatory details: For each Payer, there are some mandatory details to complete the eligibility request. If the mandatory details are missing, CharmHealth prompts the user to enter the details.

Reason: This error indicates that the selected Provider/Facility doesn't have an NPI. NPI is mandatory to check Insurance Eligibility in real-time.
Solution: Navigate to 'Settings > Practice Members' List. Edit the respective Provider and update with a correct NPI. Similarly, if it is a Facility, then update the respective Facility under the 'Settings > Facilities' section. - Missing/Incorrect Information: The Clearinghouse will respond with the benefit information if there is any matching Insurance detail for the Patient. If not, the Clearinghouse responds with an error message. The following is one such error where the Patient's name and Date of Birth (DOB) in the demographics do not match with the Payer database.

Reason: This error indicates that the Payer could not identify the Patient with the given insurance details in their system.
Solution: Verify and update the Patient's insurance details with the correct DOB/Name/Member ID details. - Timeout Error: If CharmHealth does not receive a response from the Clearinghouse within 60 seconds, a timeout error will be shown. The users can send the eligibility request after a few minutes. Refer to the below screenshot.

Reason: The above error indicates that CharmHealth couldn't connect with Optum system to check eligibility.
Solution: Please try to check eligibility after some time.