Electronic Prior Authorization
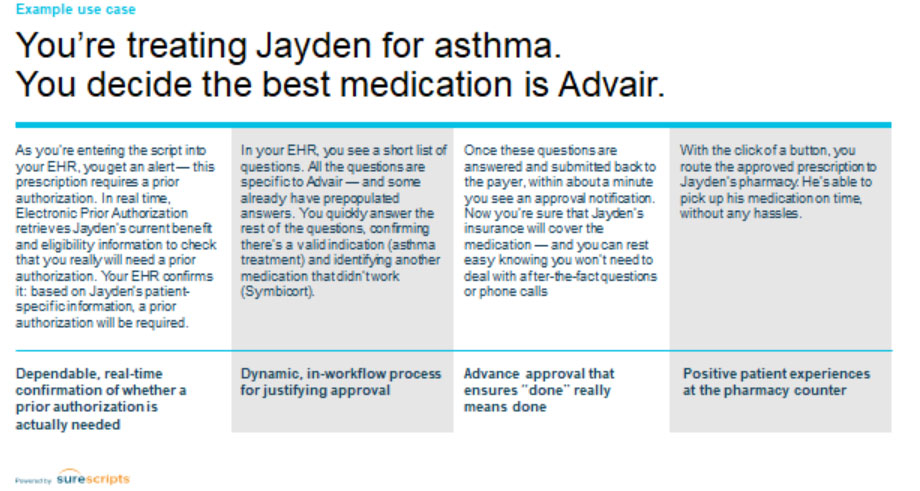
Electronic Prior Authorization helps you to streamline your workflow by making the most efficient medication-related prior authorization process by default. With the ability to identify the prior authorization process at the point of care, you will improve your Practice’s efficiency, avoid post-visit disruptions, and deliver an even more satisfying experience for patients.
How dose it works
With Electronic Prior Authorization, you will increase the efficiency, reduce disruption, and give a faster path to successful treatment of the Patient.

Electronic Prior Authorization allows you to improve and simplify your current workflow, which might look like a disruption today is ultimately an upgrade to a smoother and better process. We embed all functionality directly into your clinical EHR workflow and have prioritized features that help you avoid unnecessary work. Submit the prior authorization electronically and typically get approval within 60 seconds.
It’s powered by Surescripts that connects to more PBMs and payers than other options. Today, it is already linked to 89% of covered lives in the United States, and it is growing every year.
Advantages
- Adds a complete, guided prior authorization process into your everyday EHR workflow
- Replaces faxes and phone calls with a completely automated process
- Communicates in real-time directly with the Nation’s largest PBMs
- Covers all medication classes and specialty medications
- Streamlines the prior authorization process at the Practice level or for centralized teams
- Combines with Real-Time Prescription Benefit to transform Patients’ experiences
How EPA and RTPB Work Together
By combining a fully electronic prior authorization validation and approval process with patient-specific coverage details and medication alternatives, our solutions will improve your Practice’s efficiency, accelerate Patient time to therapy, encourage prescription adherence, and improve patient satisfaction.
Together, Real-Time Prescription Benefit and Electronic Prior Authorization eliminate barriers to better prescribing, leading to an accelerated, optimized prescription process.

Work Flow in CharmHealth EHR
Initiate electronic PA on writing the prescription
Step #1: Open an Encounter or Quick Rx view.
Step #2: Start writing a prescription using the 'Add Rx' option. Prescriptions can be also added to the chart note through other options like Templates, Past Rx, etc.
Step #3: Search the drug that you need to prescribe.

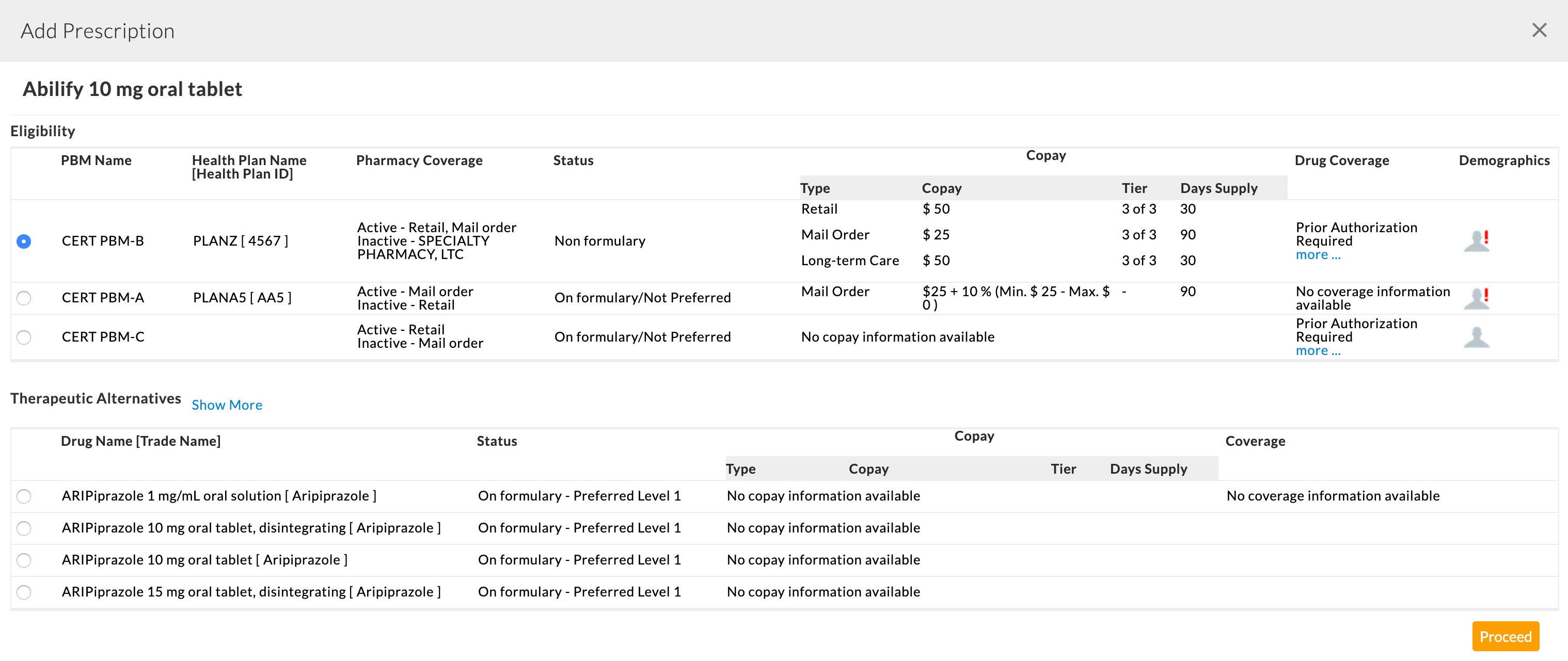
Step #4: With EPA enabled, selecting a prescription will show the formulary eligibility details of the prescription based on the Patient's insurance plan details. If PA is required for the prescription in a plan, 'Prior Authorization Required' information will be shown in the Coverage details section.
Step #5: Choosing an insurance plan takes you to the prescription view. If the eligibility response of the prescription says Prior Authorization is required, then the ‘Initiate Electronic Prior Authorization’ checkbox gets checked by default.
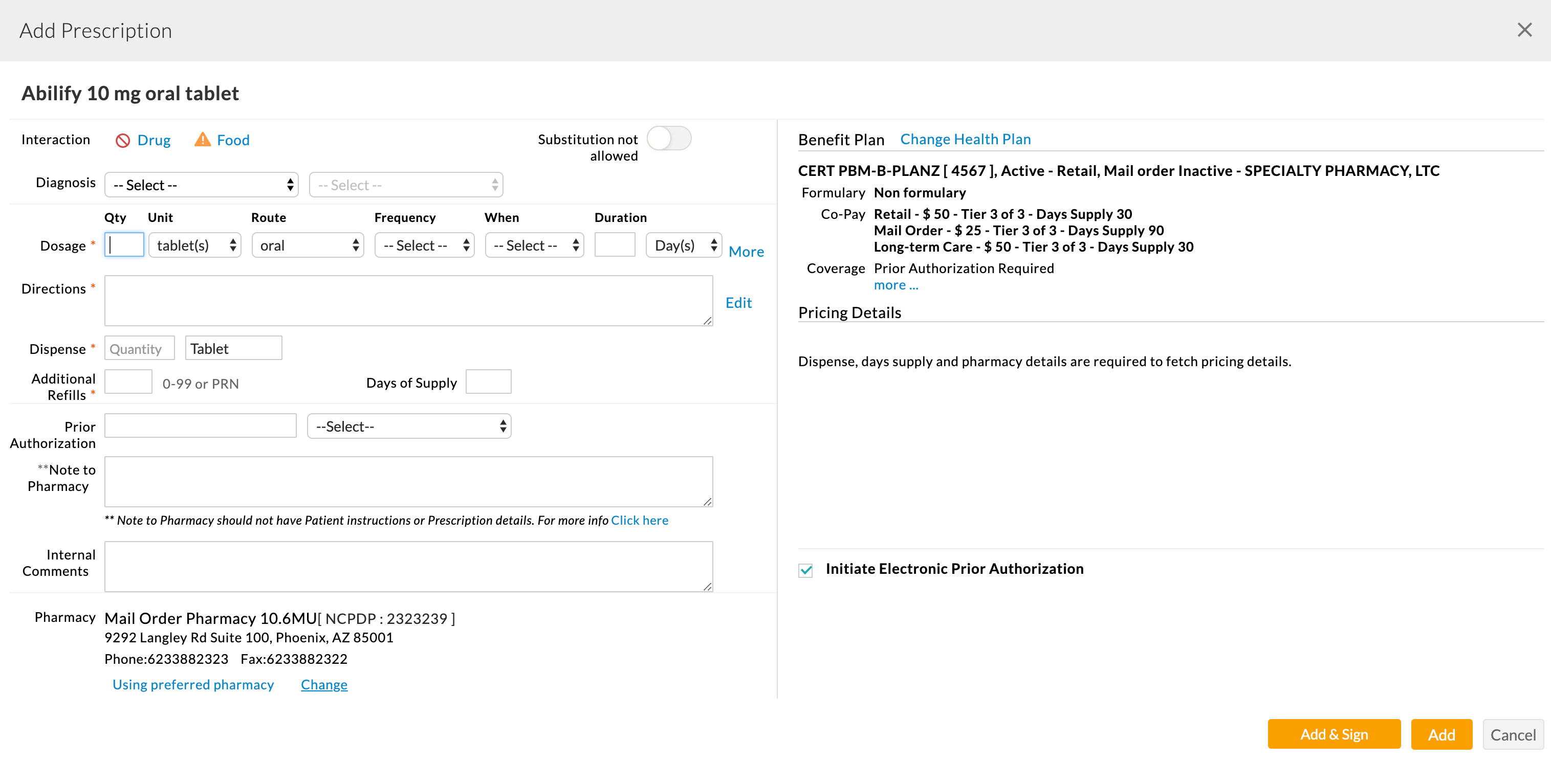
If the ‘Initiate Electronic Prior Authorization’ is not checked automatically as the eligibility response does not have a prior-auth required indicator, the Prescriber can check the ‘Initiate Electronic Prior Authorization’ option.
Step #6: Days supply, Quantity, Dispensing unit, and Pharmacy details need to be filled in. RTPB pricing and alternative details will be fetched and displayed on the right side of the view, if available.
If any of the alternatives do not require PA, the user can choose the alternative instead of the current prescription to avoid PA. The Prescriber can also uncheck the ‘Initiate Electronic Prior Authorization’ option to avoid initiating prior authorization automatically if the Prescriber knows that any particular drug does not require prior-auth based on the Patient's condition.
Step #7: Users can continue with the current medication or alternative medication that requires prior authorization. With the ‘Initiate Electronic Prior Authorization’ option in the checked state, adding the prescription to the system will automatically initiate an electronic prior authorization request to the Surescirpts - PBM services.
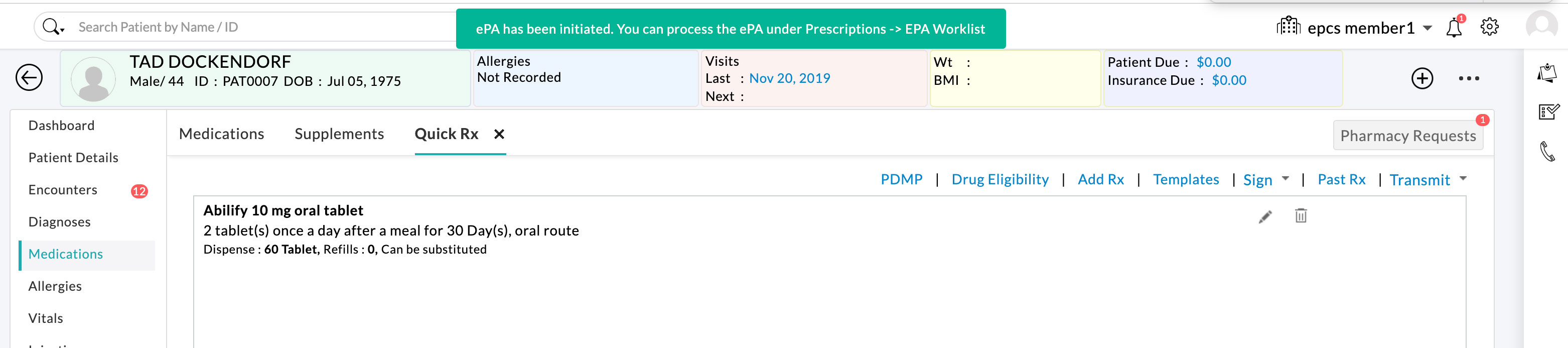
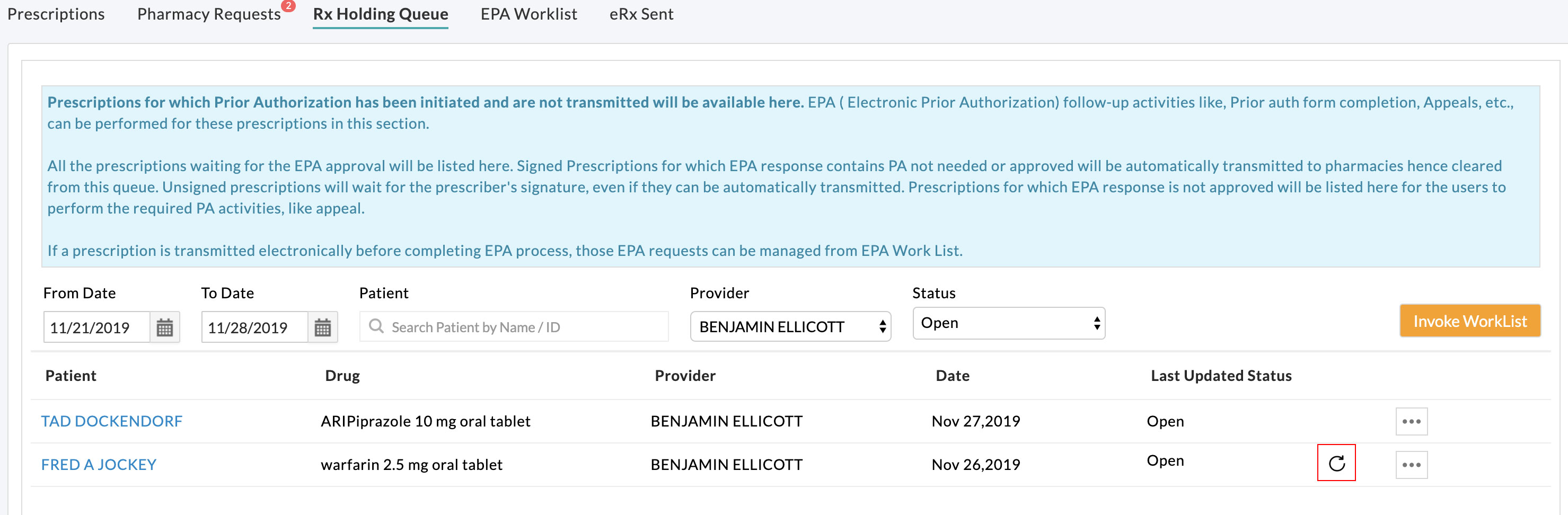
Step #8: Once EPA is initiated for a prescription, further EPA activities (like completing PA form, acknowledging, and appealing) for this prescription can be performed from the 'Rx Holding Queue' section until the prescription gets transmitted.
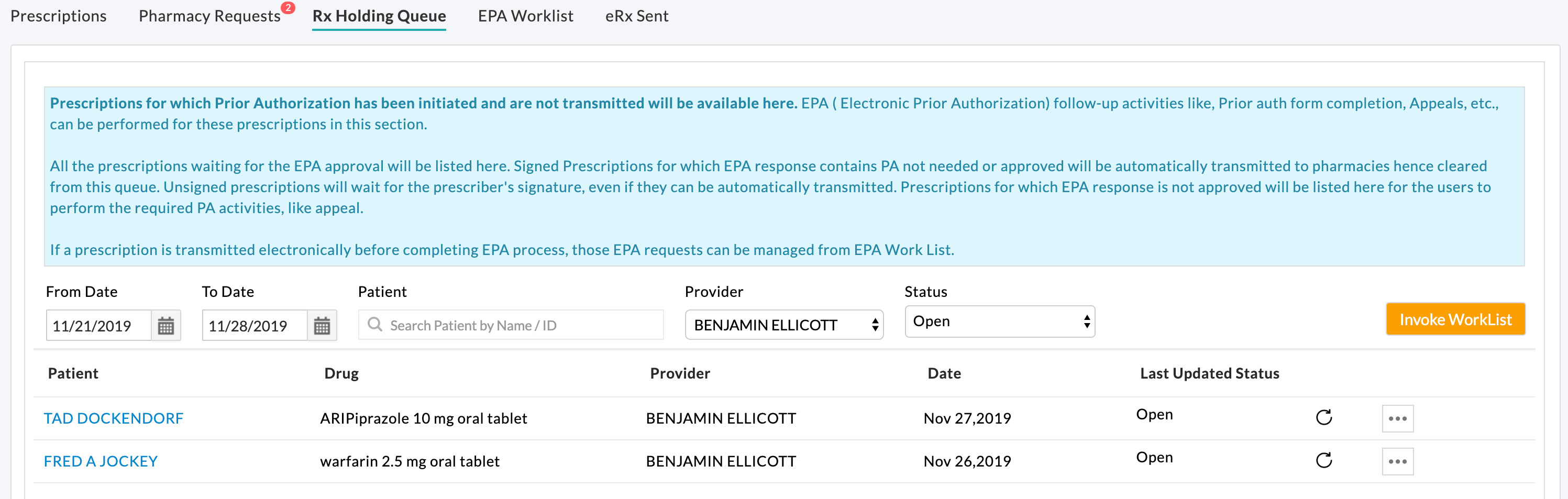
If the Prescriber needs to transmit a prescription before completing the EPA process, it can be transmitted from either Encounter view or Rx Holding Queue. Once the prescription is transmitted, the prescription is removed from Rx Holding Queue, and the EPA activities should be performed from EPA WorkList View.
Initiate Electronic PA for a Transmitted Prescription
EPA can be initiated for transmitted prescriptions from the Patient's Medication section by the Prescriber/Agent.
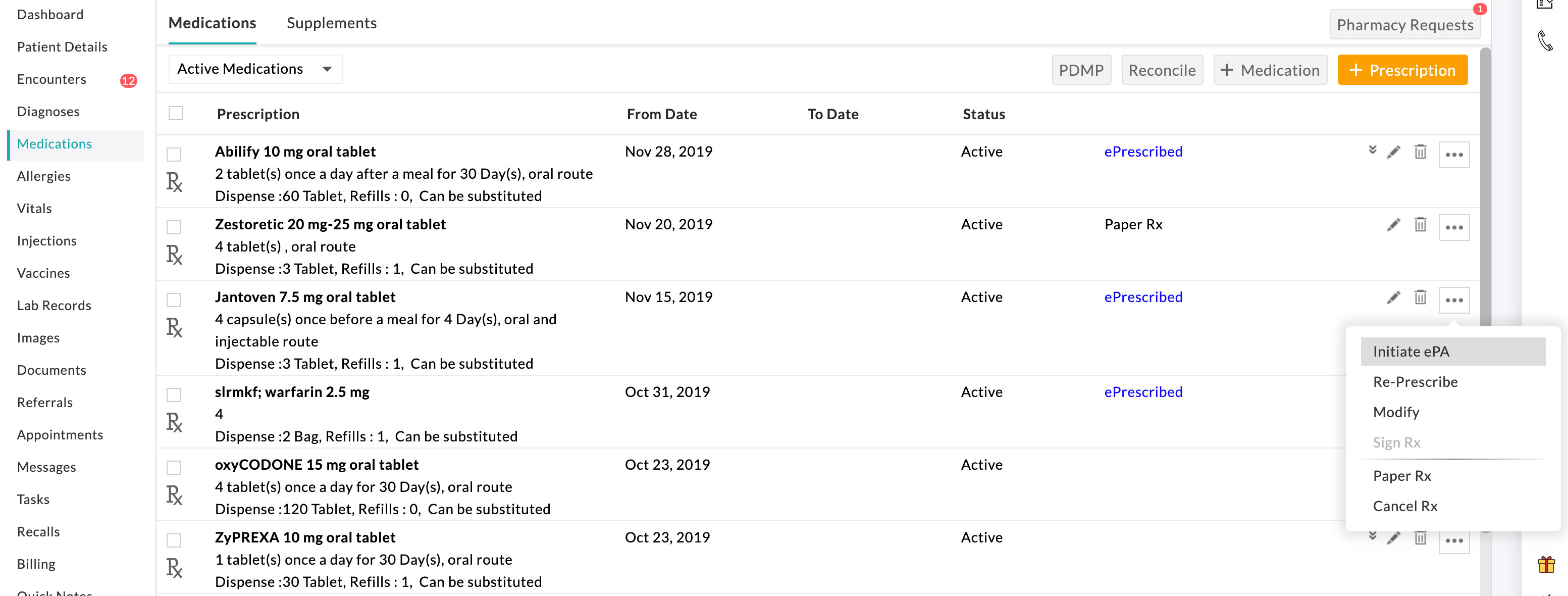
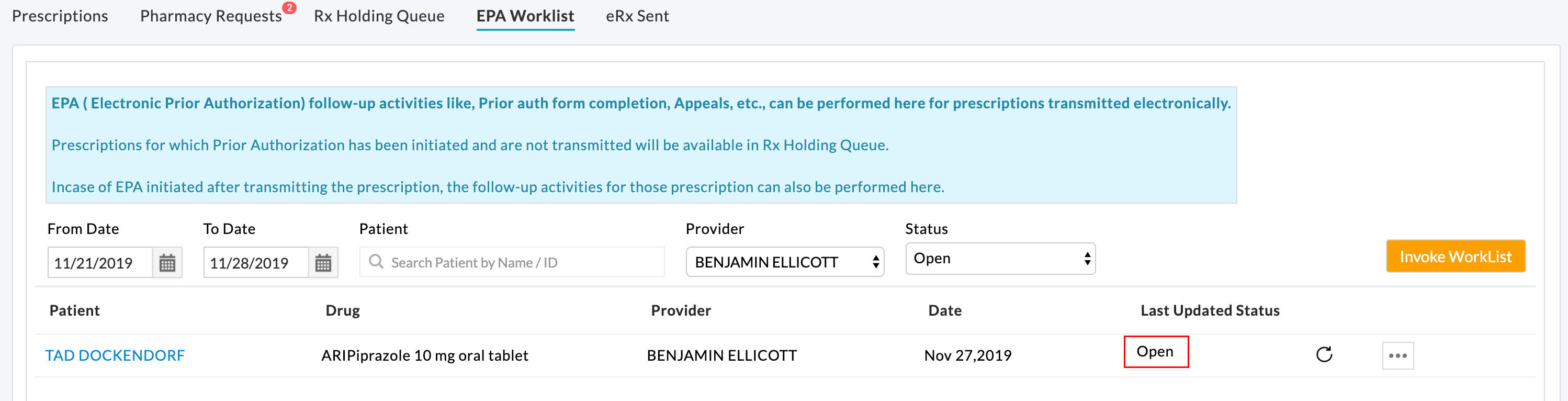
EPA activities for transmitted prescriptions can be handled in the EPA WorkList View.
EPA Activities on Prescription:
EPA status and follow-up activities can be viewed and performed for the prescriptions from either the 'Rx Holding Queue' or 'EPA Worklist' views. Rx Holding Queue view lists the prescriptions which are not yet transmitted and are awaiting EPA completion. EPA Worklist view holds the list of transmitted prescriptions involved in the EPA process.
Initiating the EPA process sends an EPA request to Surescripts. Surescripts forwards the request to the PA processor (PBM/Payer). The request is reviewed, and the response is returned with any of the below statuses to the CharmHealth EHR account. The actions needed from the user based on the received response are also mentioned in the table.
| EPA Initial Response | Action Required |
|---|---|
| Completed - PA not needed for medication/patient/health plan combination. | No action is required from the prescriber end. |
| Completed - PA not allowed, medication not covered. | This status represents PA cannot be proceed electronically. So either, A manual PA process should be followed -- Or -- Filling PA from via web-based PA forms provider |
| Open & Question Set Returned - PA allowed, please complete the attached question set. | PBM returns Question-Set which needs to be filled by the prescriber/clinical end. |
The status of the EPA process can be checked by clicking the refresh icon in the 'Last Updated Status' column.
CharmHealth EHR uses Surescripts EPA Accelerator service for EPA activities. From both Rx Holding Queue and EPA Worklist view, clicking the 'Process PA' option launches the Surescripts Accelerator UI to know the status and the actions to be performed by the user.

Users get redirected to Surescripts Accelerator UI (User Interface). This view shows the state of the workflow process, including the status of the process and context-specific details.
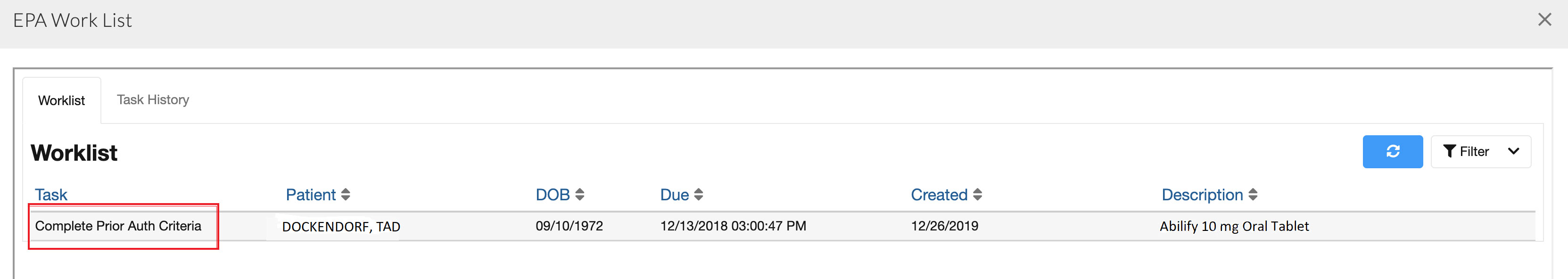
In the task history list view, some tasks may be associated with the action required from the PBM/Payer and will not require interaction from the user within the Prescriber system.
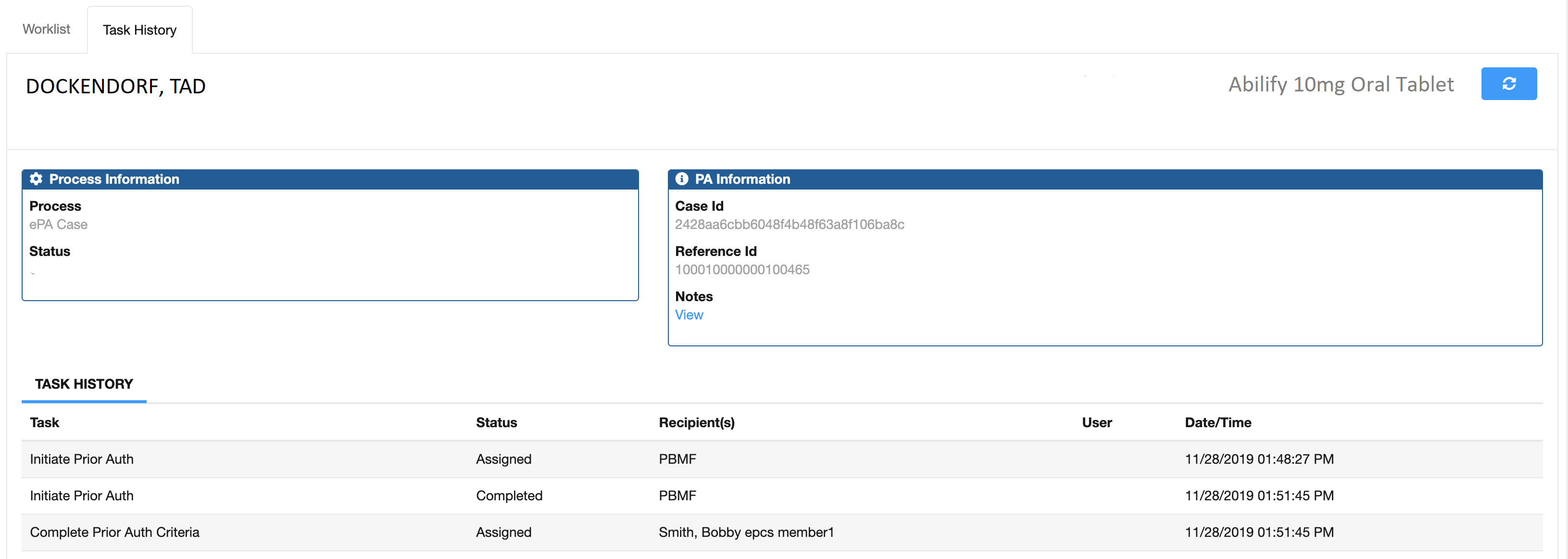
Task Names that may require action from the Prescriber (or their proxy) include: 'Complete PA Form' and 'Acknowledge' tasks (e.g. 'AcknowledgeClosedPA'). Surescript Accelerator launches a question set if the task is 'Complete Prior Auth Criteria/Form'.
Handling of EPAs returned with Question Set
Opening the 'Complete Prior Auth Criteria' task opens up the question sets with the answering process view.
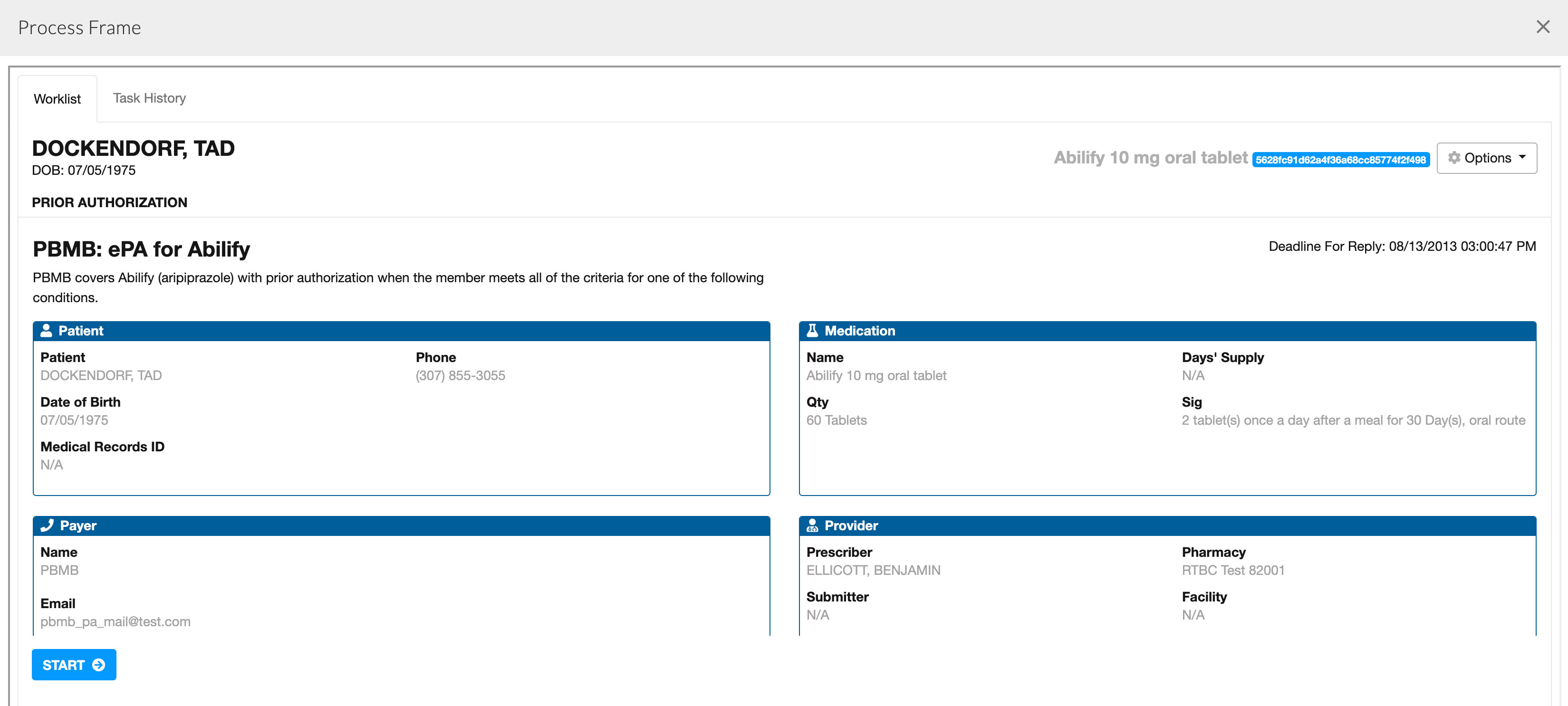
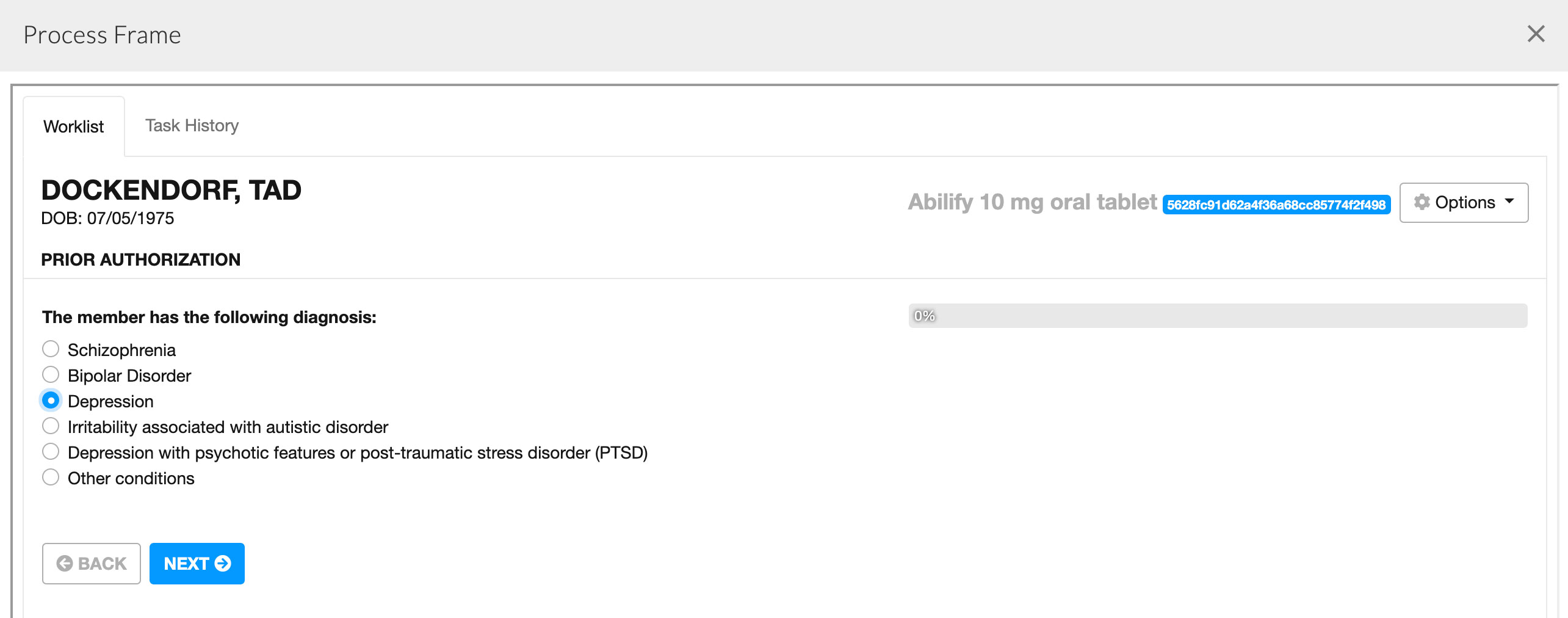
PA form questions need to be filled with the appropriate answers for quicker approval of PA. The PA form can be submitted at the end of answering the question sets. These answers will be sent to PBM, and wait for PBM response.
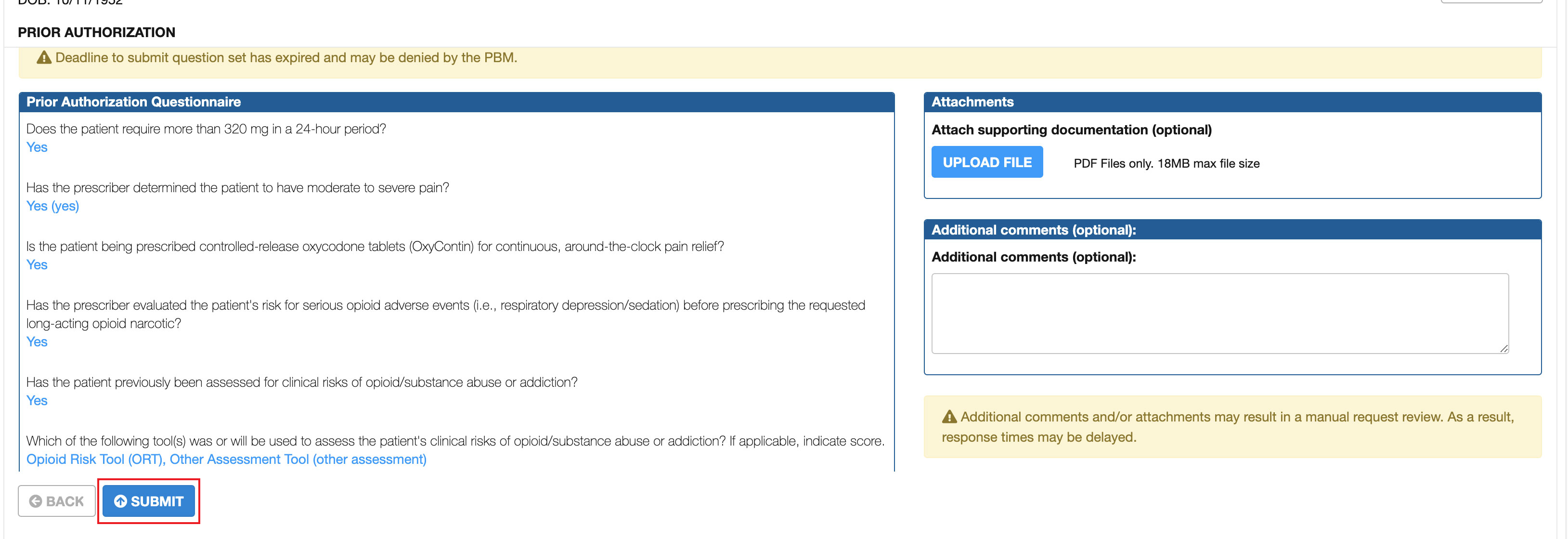
After submission, the task gets assigned to PBM for processing the complete PA form. The PBM (or health plan) will review the answer set and approve or deny the Electronic PA based on the responses to the question set.
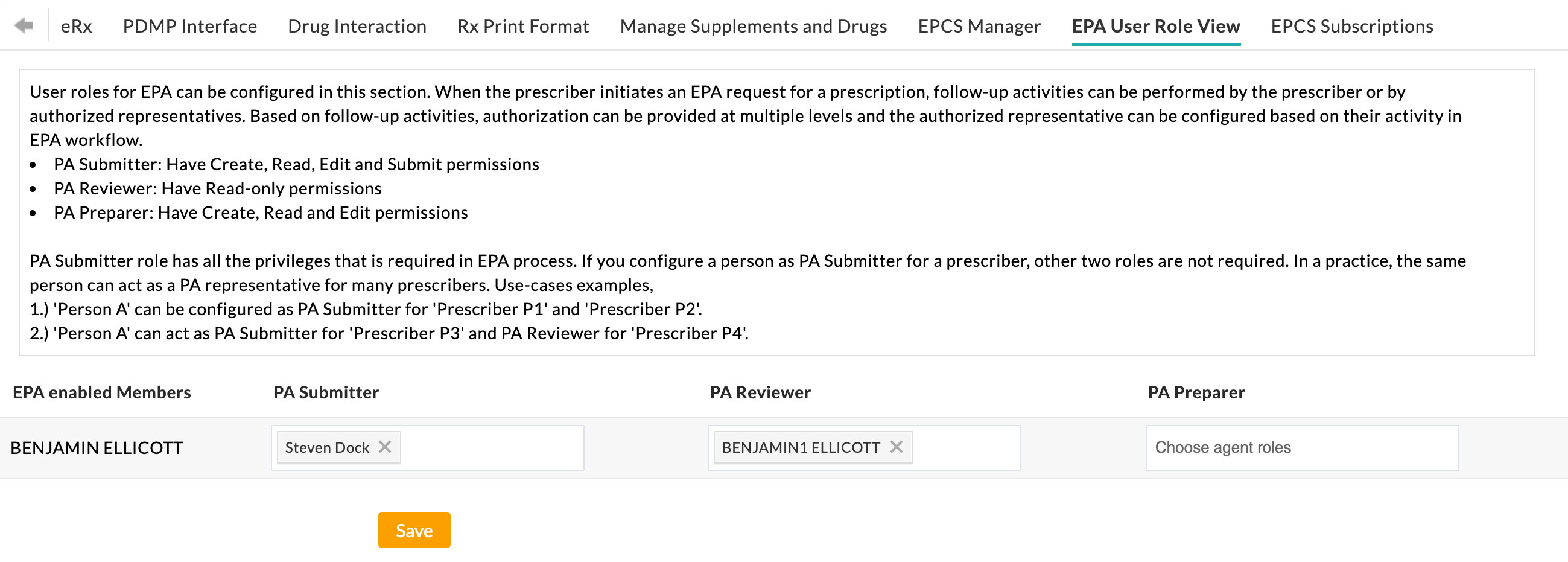
Approved EPA Worklist:
If the PA is approved by PBM, the status of the PA is updated to 'Approved' in the Work List view.
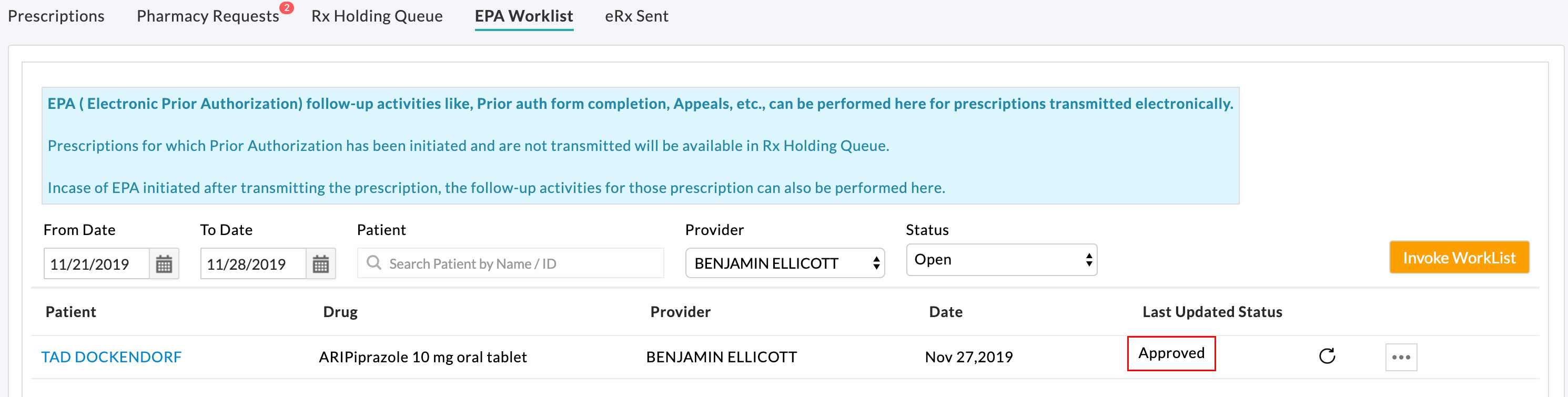
If the signed prescription is not yet transmitted and available in the 'Rx Holding Queue,' the prescription can be transmitted electronically to the Pharmacy.
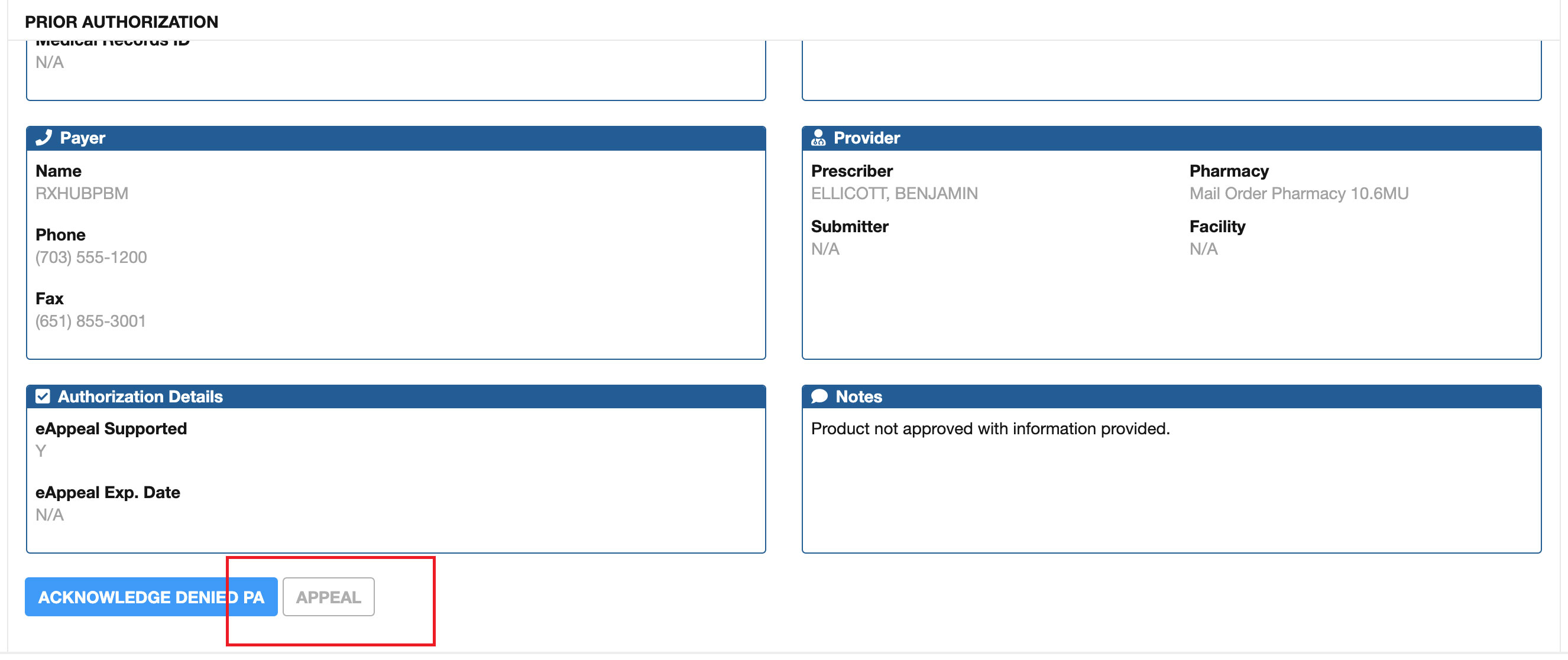
Denied EPA Worklist:
If the PA is denied by PBM, the status of the PA is updated to 'Denied' in the worklist view.
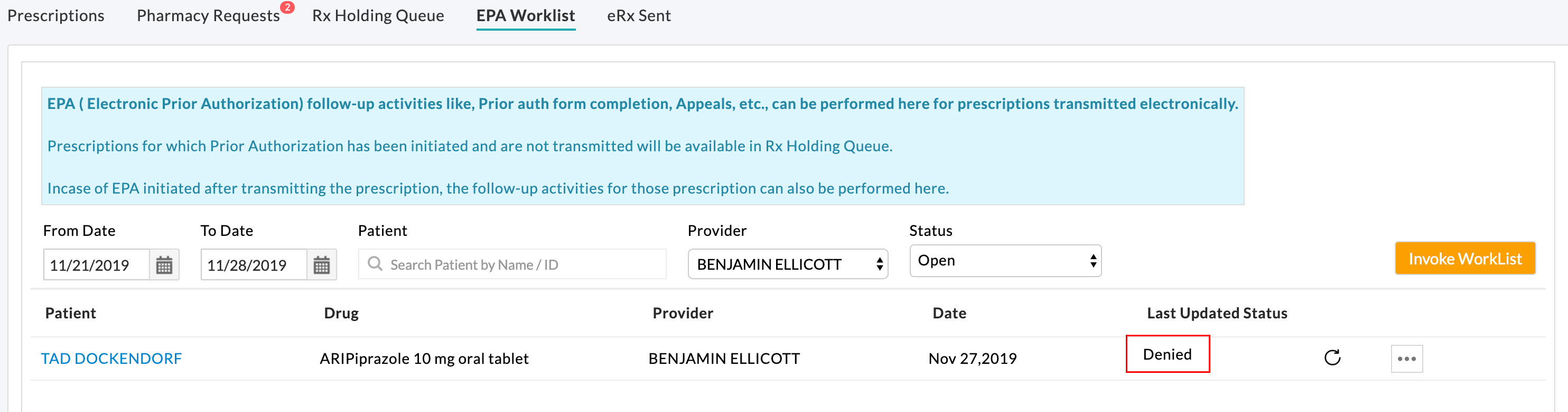
For denied electronic PA, there may be an option to submit an electronic appeal if the PBM or health plan supports the message type for this medication/health plan combination.
Handling of EPAs with status 'Completed - PA not needed':
In this scenario, Surescripts Accelerator UI displays the worklist with the 'PA Not Needed' task. No further EPA-related action is required from the Prescriber/Clinical end.
If the signed prescription is not yet transmitted and available in the 'Rx Holding Queue', the prescription can be transmitted electronically to the Pharmacy.
Handling of EPAs with status 'Completed - PA not allowed':
Scenario #1:
Matching the information within the PA-Initiation-Request to a single PA form is generally not possible. The matching process typically results in multiple matches or no matches. This is largely due to information such as BIN/PCN, Group IDs, and Plan IDs being used by multiple plans across several different PBMs.
In instances where Surescripts is not able to return a PA Form, the following will be received in a Closed - Other message.
Sorry but Surescripts cannot process this PA request electronically. Please refer to the back of the Patient benefit card for information on how to process this prior authorization manually.
What to do next?
Users can send the medication to the Pharmacy. If a PA is needed, the Pharmacy will notify the Clinic, and a manual process should be used to ensure that the Patients’ needs are addressed.
Scenario #2:
When Surescripts is not able to find an electronic path to complete a prior authorization, it will default to a PDF workflow to identify and return a PA form for the user to complete the PA.
What to do next?
The user should be directed to act on the PDF URL by clicking the hyperlink. A portal will get opened with a prepopulated PA form for the user to complete. PDF URLs will be active only for 72 hours.
Once the user fills out the PA form provided by the web-based PA forms Provider, the form is faxed to the PBM/Payer, and there will be no further electronic communication to the EHR by either the web-based PA forms Provider or Surescripts. The PBM/Payer will fax the Provider vendor back the approval or denial.
Rx Holding Queue and EPA Status Scheduler
Rx Holding Queue view lists the prescriptions that are not yet transmitted and awaiting EPA completion. CharmHealth EHR runs an EPA Status Scheduler at regular intervals to check the status of EPAs in progress. If the EPA status is approved or 'PA Not Needed,' our EPA Status Scheduler checks the status of the related prescriptions to automatically transmit them to the Pharmacies electronically. Prescriptions already signed by the Prescribers get automatically transmitted to the Pharmacies without any user intervention and get cleared from Rx Holding Queue. If the prescriptions are not yet signed by the Prescriber, those prescriptions are listed in the Rx Holding Queue to be signed by the Prescriber for transmission.
On transmitting NewRx electronically, prior-auth status and details are sent as a part of the prescription script to the Pharmacy if the PA is processed electronically. Else if the PA is processed manually, the user can fill in the PA details manually in the prescription view before transmitting to the Pharmacy to make the PA details part of the prescription script.
Re-initiate EPA
EPA can be re-initiated for the prescriptions without any outstanding EPAs in progress from the Patient's Medication section by the Prescriber/Agent.
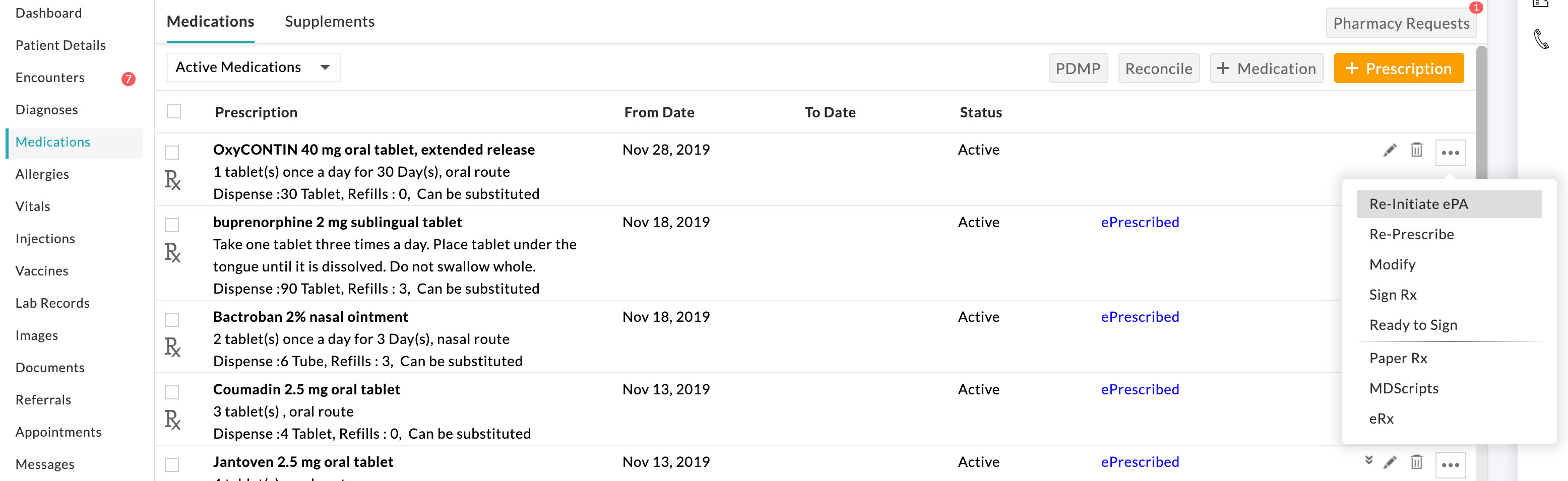
Re-initiate EPA opens up the prescription view with EPA History details for reference.
The benefit plan can be changed, and the EPA can be re-initiated. Re-initiated EPA follow-up activities can be followed up from Rx Holding Queue if the prescription is not yet transmitted. If the prescription is already transmitted, EPA activities can be performed from the EPA Work List.
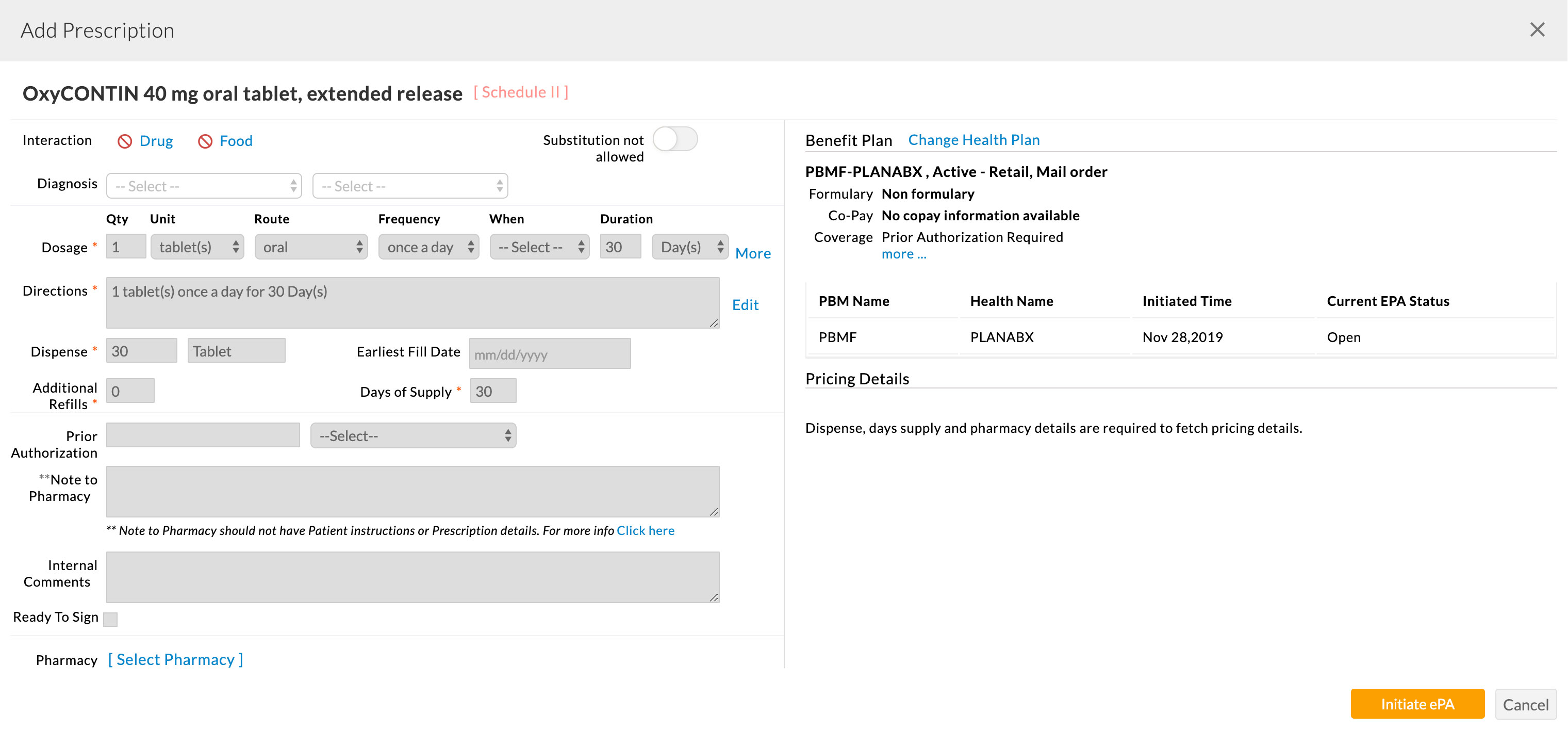
Configuring Authorized Representative for EPA Activities
When the prescriber initiates an EPA request for a prescription, EPA follow-up activities can be performed by the Prescriber or authorized representatives. Based on the follow-up activities, authorization can be provided at multiple levels, and the authorized representative can be configured based on their activity in the EPA workflow.
- PA Submitter: Have Create, Read, Edit, and Submit permissions.
- PA Reviewer: Have Read-only permissions.
- PA Preparer: Have Create, Read, and Edit permissions.
The PA Submitter role has all the privileges that are required in the EPA process. If you configure a person as PA Submitter for a Prescriber, the other two roles are not required. In Practice, the same person can act as a PA representative for many Prescribers. A few use cases are given below for better understanding,
- 'Person A' can be configured as a PA Submitter for 'Prescriber P1' and 'Prescriber P2'
- 'Person A' can act as a PA Submitter for 'Prescriber P3' and PA Reviewer for 'Prescriber P4'
An authorized representative can perform the EPA-related activities on behalf of the associated Prescribers from EPA Work List or Rx Holding Queue views.
EPA Work List & Rx Holding Queue view list all the EPAs for the prescriptions written by the associated Prescribers. Users can apply filters to refine the EPAs on which they have to work.
User's Actionable Tasks on In-progress EPAs
The 'Invoke WorkList' button in the Rx Holding Queue/EPA Work List view helps the user by listing the EPAs requiring action from the User/Prescriber end.
Users can view their EPA actionable tasks in the Surescripts Accelerator Worklist view.
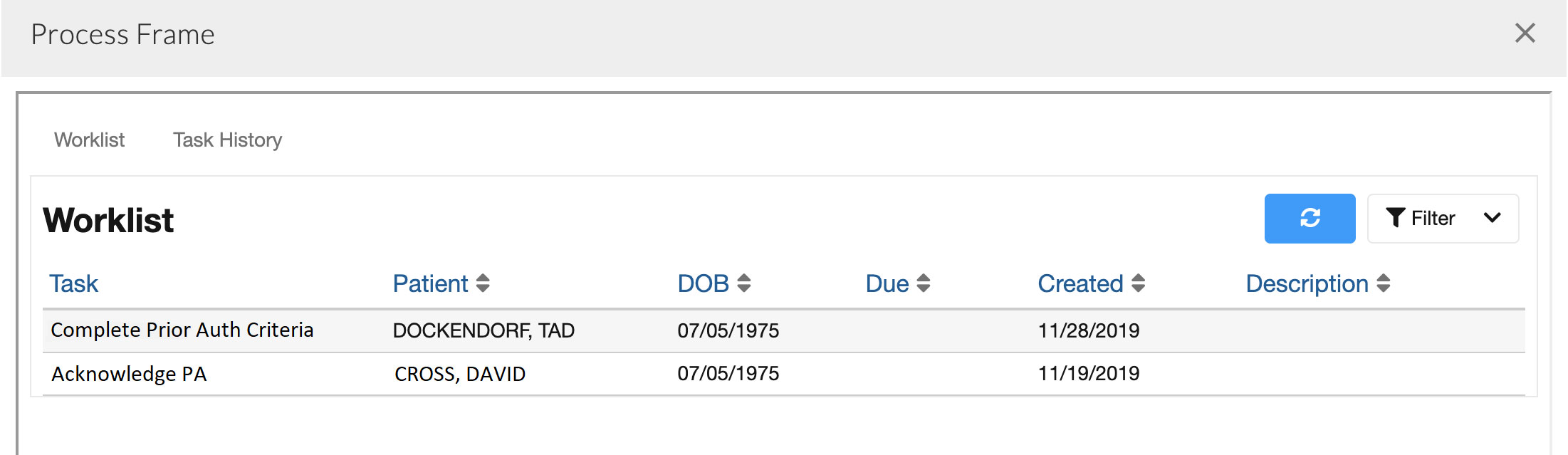
The user may select a task and trigger the Accelerator to go to the appropriate view for that task. Tasks related to EPA are assigned to the recipient of the EPA Message, e.g. the Prescriber who has initiated the EPA request. The users can take action on the tasks. The EPA process may get completed on performing a task, or a new task may get created which requires additional action from the PBM side to complete the EPA process.