Invoices
- Generate Invoice
- Automatic Invoice Generation and Settings
- Invoice Actions
- View Invoice Details
- Edit the Approved Invoice - Edit Invoice
- Add Payment to the Invoice - Add Payment
- Update/Adjust posted Payment - Adjust Payments
- Send Invoice to a Patient
- Setting to Allow Partial Payment for 'Invoices' and 'Statements' Sent to the Patient
- Mark Invoice as Mailed - For Physical Copies
- Print and Download Invoice
- Mark/Unmark the Invoice to 'Sent for Collection Agency'
- Add Notes to Invoice
- Flag/Un-flag the Invoice
- Cancel Invoice
- Delete the Draft Invoice
- Handling Non-Covered/Self-Pay services
- Add Procedure Code to Multiple Invoices
- Associating Products with the Procedure Codes
- Associating Procedure Codes with Lab Tests
- Send Multiple Invoices to Patients
- Claim Generation
- Bulk Actions on Invoices
- Handling 'Credit Notes'
- Handling Refunds
- Invoices - Watch List
- Usage of 'Date Range'
- Using 'Search Options 1' and 'Search Options 2'
- Sorting option on 'Invoices List View'
- Details of Icons (Insurance/C/Card/Credit Note/etc.) shown in 'Invoices List View'
- For Practices Working with CharmRCM or CharmBillerPro
- Invoices - Reports
- Preferred settings for cash based practices
- Preferred settings for cashless practices
- Hard Closing of Accounts
Generate Invoice
Generate Invoice for an Encounter
To generate an Invoice for an Encounter, follow the steps given below.
- Navigate to the Billing > Generate Bills section.
- Click the 'More Options' (...) icon against the Encounter and select the 'New Invoice' option.

- Select the respective Encounter in the 'Encounter Date' field. Once it is selected, Procedures/Drugs/Supplements will be auto-populated in the Invoice.
- New Procedures and Products can be added to the Invoice using the inline 'Search & Select' option. You can choose the Procedures/Products from the 'Choose from Master List' or 'Choose from Templates' options.

- Select the applicable taxes for Products. If default Tax is configured for the Procedures/Products, it will be auto-populated.
- Default Charge and Discount (configured in Settings) will be auto-populated. If required, you can update the Charge and Discount.
- If Credit is available for the Patient, you can use the credit for the Invoice by selecting the 'Adjust the available patient credits against the Invoice' option.
- In the 'Payment Details' field, choose the Payment options. If you are collecting full payment for the Invoice, you can make use of the 'Pay Invoice in full' option. This will auto-populate the amount in the 'Payment Amount' field. If the default 'Payment Method' is configured, it will be auto-selected in the Invoice.
- If default 'Notes' and 'Terms & Conditions' are configured in the settings, they will be auto-populated in the Invoice. If required, you can update these details specific to the Invoice.
- You can add the Provider Signature under the 'Settings > Encounter > Signature' section. You can draw the signature on a Signature Pad or upload a picture of your signature from your computer. Select the 'Billing - Invoice PDF' option to include the Provider Signature in the Invoice.
- To enable Patient Signature in the Invoice Summary, go to 'Settings > Billing > Billing Settings > Invoice Settings - Additional Options'. Select 'Yes' for the 'Enable patient signature in invoice summary' option.
- Click the 'Approve' button to get the Invoice approved.
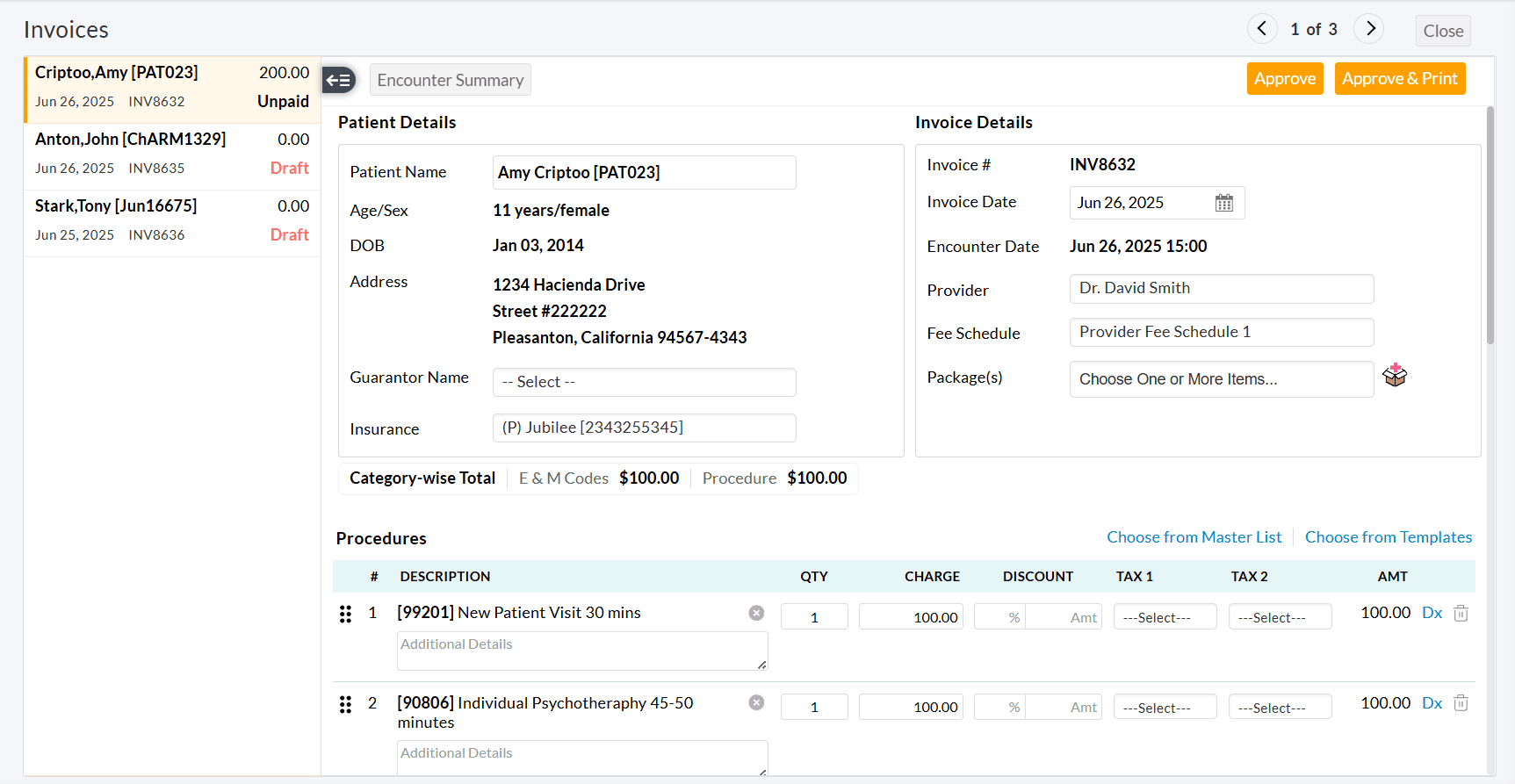
Generate Invoice without Encounter
- Navigate to the Billing > Invoices section.
- Click the '+Invoice' button to create an Invoice.

- Enter the Patient name for whom you need to generate an Invoice.
- To generate an Invoice without Encounter, you don't need to select any option in the 'Encounter Date' field. Select the applicable Provider for the Invoice.
- If a Package is available for the Patient, you need to select the required Package to use the item from that Package.
- If a 'Fee Schedule' is configured for this Provider/Patient, it gets auto-selected by default. The Charges/Discounts will get auto-populated for Procedures/Products as per the 'Fee Schedule'.
- Search and select the Procedures/Products in the line items along with their charges and discounts.
- Select the Payment details and click the 'Approve' button to generate the Invoice.
Generate Invoice with Bluefin Payment
Practices can make transactions through the Bluefin payment gateway while generating the Invoice.
- Navigate to 'Billing > Invoices'
- Click the '+ Invoice' button to create an Invoice. You can also create an Invoice for an Encounter under the 'Generate Bills' section.
- Add the Procedures or Products to the Invoice.


- Select the 'Use Payment Gateway' checkbox and specify the Payment Amount and Payment Method.
- Choose the 'Beneficiary' account to which the amount should be credited.
- The following settings can be configured as a default value under the 'Settings > Billing > Bluefin > Default Settings' section.
- The Patient address can be auto-populated as the Cardholder address.
- The Input Type for Bluefin payment can be set to default. This input type gets automatically selected when choosing Bluefin as a beneficiary account while adding or adjusting payments.
- While adding Payment, choose to keep the 'Store card details in Payment Gateway' option selected by default.
- You can also set the default 'Payment Method' under the 'Settings > Billing Settings > Receipt Settings > Default Payment Method' section.
- Click the 'Approve' button to approve the Invoice and initiate the transaction through the payment gateway.
- Upon successful transaction, the Invoice status will change to 'Paid' or 'Partially Paid' based on the amount paid, and the Receipt gets generated for the Invoice.

Note
- When 'Payment Gateway' is used, the Invoice cannot be saved as a Draft.
- This 'Use Payment Gateway' option will be shown only for the Practices with Bluefin Payment Gateway integration.
Save or Approve the Invoice
To save the Invoice as a draft, follow the steps given below.
- On creating an Invoice, click the 'Save as Draft' button as shown in the screenshot.

- The Invoice gets saved as a draft and can be edited anytime later from the 'Billng > Invoices' section.

- To approve the Invoice, click the 'Approve' button.
- To approve and print the Invoice, click the 'Approve & Print' button.
Important Invoice Settings
You can configure the Invoice Settings under 'Settings > Billing Settings > Invoice Settings'.

- Choose whether to auto-select the Primary Insurance of the Patient in the Invoice under the 'Invoice Generation- General Settings' section.
- Option to auto-adjust the available Patient credits against the Invoice while invoicing under the 'Invoice Generation- General Settings' section.
- Option to auto-select either the first Dx code or the first four Dx codes for all Procedure codes. A maximum of four Dx can be auto-associated with the procedure codes. You can also choose not to auto-select the Dx pointers. You can configure this setting under the 'Invoice Generation - General Settings' option.
- Choose the default auto-payment options viz., Pay Invoice in full, Pay Products in full, Pay Co-pay, and Pay Non-Covered Services while generating an Invoice and as well as while adding payments under the 'Invoice Settings - Default Options' section.
- Enter the alternate names for Invoice, Procedure Table, and Products Table under the 'Invoice Settings -General' section.
- Configure default Notes and Terms & Conditions under the 'Invoice Header and Notes Configuration' section.
Additional Options for Inventory-enabled Practices
If the Practice has its own Inventory module, the following settings can be configured.

- Choose 'Yes' for the 'We use Inventory module and dispense products' option if you have your Inventory and dispense your Products.
- Whether to auto-populate the Drugs and Supplements details in the Invoice from the Encounter. You can also choose to select either the Drugs or Supplements to auto-populate.
- Whether to auto-populate the Dispense quantity of Drugs & Supplements in the Invoice from the Encounter. If the option 'Yes' is selected, the dispense quantity of the Drugs & Supplements from the Encounter gets auto-populated while generating an Invoice.
- Whether to auto-populate the 'Dispense Quantity' in the Invoice only for Drugs/Supplements having 'Dosage Unit' as tablet(s), capsule(s), caplet(s), or pellet(s). If the option 'Yes' is selected, the dispense quantity only for the Drugs & Supplements with the Dosage Unit from the Encounter gets auto-populated while generating an Invoice.
Automatic Invoice Generation and Settings
CharmHealth allows the Practice to generate the Invoice automatically for an Encounter. To enable this feature, follow the steps given below.
- Go to the 'Settings > Billing Settings > Invoice Settings > Invoice Generation - General Settings' section.

- Opt to choose 'Yes' for the 'Enable Invoice Automation' option.
- Choose when to generate an Invoice automatically.
- Once the Encounter is signed and/or,
- At the end of the day.
- Automate Invoice generation only when the procedures are available in the Encounter or procedures and/or products are available in the Encounter.
- Choose whether to automate Invoice generation for all Providers or specific Providers.
Invoice Actions
View Invoice Details
To view the Invoice details, follow the steps given below.
- Go to the 'Billing > Invoices' section.
- Click the 'More Options' (...) icon against the Invoice you need to see the details.
- Select the 'View Details' option.

- A summary of the Invoice gets displayed.

Edit the Approved Invoice - Edit Invoice
To make any changes to the approved Invoices, follow the steps given below.
- Go to the 'Billing > Invoices' section.
- Click the 'More Options' (...) icon against the Invoice you need to edit.
- Select the 'Edit Invoice' option.

- For an already approved Invoice, the Claim will be available. In this case, any change in the Procedure details will automatically reflect in the Claim.
- Update the details and click the 'Approve' button.
Add payment to the Invoice - Add Payment
To add payment details and to collect the Co-pay from the Patient, follow the steps given below.
- Go to the 'Billing > Invoices' section.
- Click the 'More Options' (...) icon against an Unpaid Invoice.
- Select the 'Add Payment' option.
- Enter the Payment Amount and Payment Method. If you are using Bluefin Payment Gateway, enable the 'Use Payment Gateway' option.
- In the 'Payment From' drop-down, choose the entity responsible for the payment: Primary Payer, Secondary Payer, or Patient.

- Select the Beneficiary Input Type and enter the Card details.
- Enter the Adjustment, Patient Responsibility, and Write-off, if any.
- Click the 'Add' button to add the payment.
Update/Adjust posted Payment - Adjust Payments
The Unused payment can be adjusted against the current Invoice and a discount can be provided under Write-off. You can adjust the payment and edit the write-off against the paid Invoice by following the steps given below.
- Navigate to Billing > Invoices
- Click the 'More Options' (...) icon against the paid Invoice.
- Select the 'Adjust payments' option. The Receipts of the Invoice get listed.

- Click the 'Edit' option against the payment.

- Adjust the payment and click the 'Update' button.
Send Invoice to a Patient
Practices can send an Invoice to a Patient to collect payments by following the steps below.
- Go to the 'Billing > Invoices' section.
- Select the Invoice to be sent to the Patient.

- Click the 'Send Invoice' button. You can also select the 'Send Invoice' option under the 'More Options' (...) icon against the Invoice.

- You can send the Invoices through multiple modes to the Patient, viz., PHR, Email, or Cell Number (Text Message). By default, the Patient's available mode(s) will be selected under the 'Send through Selected Modes' section.

- Select the 'Send Payment Link' option to enable Patients to make Invoice payments using the payment link received through Email/SMS. For Patients with PHR, a 'Pay' option will be available in their accounts. This option will be selected automatically if the Bluefin setting is enabled for the Practice.
- Choose the Beneficiary to which the amount has to be credited. You can request either the Invoice due amount or the Copay amount from the Patient's Insurance. If the Copay amount is unavailable from the Insurance, you can request the Invoice due amount.
- Enter the Subject and choose the Invoice Format to be sent.
- Edit the message content for the required mode(s) if needed.
- Click the 'Send' button to send the Invoice to the Patient.
- You can view the sent Messages under the 'Messages tab > Sent folder' section.
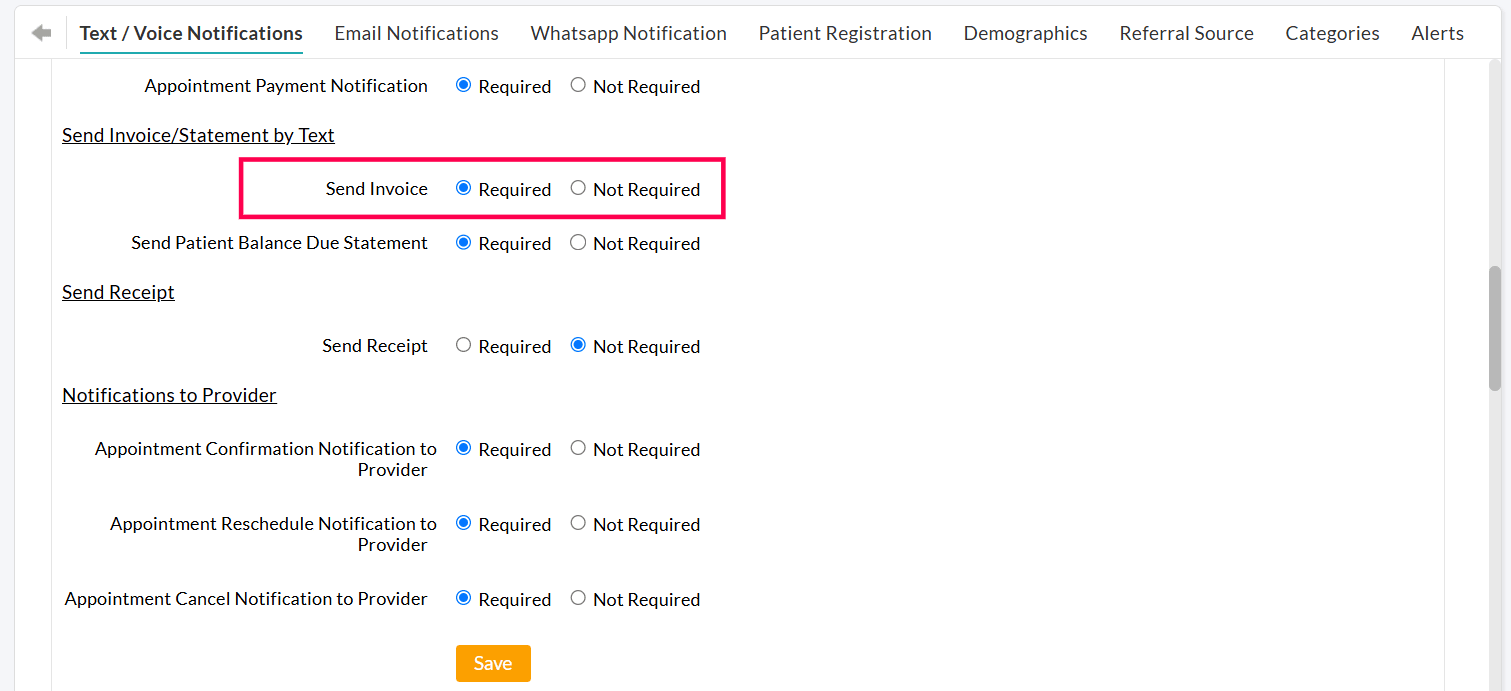
The 'Send to Cell number' option will be enabled only for the Practices subscribed for the 'Text/Voice Notification' add-on. Practices can disable this option from the 'Settings > Patient > Text / Voice Notifications > Send Invoice / Statement by Text' section.
Setting to Allow Partial Payment for 'Invoices' and 'Statements' Sent to the Patient
Practices can allow Patients to make partial Payments for Invoices and Patient Statements, providing more control and convenience in settling outstanding balances. This configuration can be enabled from the 'Settings > Billing > Bluefin > Default Settings' section.

When this setting is enabled, Patients will have the ability to modify the Total Payment Amount in the Email link, Patient Portal, and mPHR accounts.
Payment link Sent Through Email

PHR Portal

mPHR

Mark Invoice as Mailed - For Physical Copies
The physical copies of the Invoices sent to the Patients can be 'Marked as Mailed' by the Practice by following the steps given below.
- Go to the 'Billing > Invoices' section.
- Click the 'More Options' (...) icon against the Invoice and select the 'Mark as Mailed' option.

- Choose the Mailed Date and Mailed By options. By default, the address of the Patient gets filled into the 'Mailed To' field. Enter the Comments, if any.
- Click the 'Mark As Mailed' button.
- You can select multiple Invoices and mark them as mailed by clicking the 'Mark As Mailed' option under the 'Actions' button. The respective Patient's address will be taken as the mailed address.

Print and Download Invoice
Printing and downloading Invoices can be done in a specific format by choosing the appropriate format from the 'Print' and 'Download' drop-down buttons.
- Superbill PDF
- Invoice PDF
- Invoice PDF for Double Window Envelope

It applies to bulk printing where one can choose to open a single Invoice in the desired Template and get the Invoice printed.
Mark/Unmark the Invoice to 'Sent for Collection Agency'
The 'Sent for Collection' option enables tracking Invoices forwarded to collection agencies from the Practice.
Follow the below steps to send an Invoice to the collection and mark the Invoice as 'Sent for Collection'.
- Go to the 'Billing > Invoices' section.
- Click on the 'More Options' icon against any Invoice and select the 'Send for Collection' option.

- The Invoice# column indicates all the Invoices marked as 'Sent for Collection' with a small icon.
- You can also select multiple Invoices, click the 'Actions' button and choose the 'Sent for Collection' option, which marks all the selected Invoices in bulk.

- You can view the list of Invoices sent for collection using the 'Is Invoice Sent for Collection' filter under the 'Billing > Invoices > Invoices Search Options' drop-down.

- Invoices under the Sent for Collection option remain undisclosed when the Practice forwards a Patient's account statement. On clicking the 'Select All' check box, automatically uncheck the Invoices under the collection list.

Add Notes to Invoice
The Practice can add Notes to the Invoices to track or refer to them in the future. Follow the steps given below to add Notes to an Invoice.
- Go to the 'Billing > Invoices' section.
- Click the 'More Options' (...) icon against the Invoice and select the 'Add/View Notes' option.

- Enter the notes and click the 'Add' button. The Invoices with Notes are labeled with the 'Notes' tag below the Invoice Date. If there are any Past Notes added to the Invoice, it get listed under the 'Past Notes' field.

- You can filter the Invoices with Notes by using the 'Has Notes' filter option under the 'Search Options'. Choose the 'Has Notes' option from the drop-down menu.


Flag/Un-flag the Invoice
The Practice can flag the important Invoices that need further analysis/work. The Invoice can be flagged/un-flagged by following the steps given below.
- Go to the 'Billing > Invoices' section.

- Click the 'Flag' icon against the Invoice to flag it.
- You can un-flag by clicking the flag icon again.

- To filter the flagged and un-flagged Invoices, select the 'Is Invoice Flagged' option under the 'Search Options' filter. Choose the 'Flagged' or 'Un-flagged' option from the drop-down to list the respective Invoices.
Cancel Invoice
If there is no partial payment on an Invoice and no write-off then the Practice can cancel the Invoice. To cancel the Invoice, follow the steps given below.
- Go to the 'Billing > Invoices' section.
- Revert all the payments/adjustments/write-offs using the 'Adjust Payments' option.

- Click the 'More Options' (...) icon against the Invoice and select the 'Cancel Invoice' option.

- Enter the comments and click the 'Ok' button. The Invoice gets labeled with the 'Cancelled' tag, and the status gets changed to 'Cancelled'.

Delete the Draft Invoice
To delete a draft Invoice, follow the steps given below.
- Go to the 'Billing > Invoices' section.
- Click the 'More Options' (...) icon against the draft Invoice to be deleted.

- Select the 'Delete' option. The draft Invoice gets deleted from the list.
Handling Non-Covered/Self-Pay services
- Non-covered procedures can be pre-configured while adding Procedure Codes under the 'Settings > Billing > Procedure Codes' section.
- Click the '+ Procedure Code' button. Choose the Category 'Non-Covered Services' from the drop-down list and add the non-covered procedure code.
- The Practice can add the non-covered services rendered to the Patients under 'Billing > Invoices'.

- Create an Invoice and search and select the pre-configured Non-covered services under the 'Procedures' field.
- The sum of non-covered services will be shown in the 'Category-wise Total' section. This will help you to quickly check the 'Total' of all non-covered services in the Invoice.
- Select the 'Pay Non-covered' option under the Payment Details. This option can be selected by default under the 'Settings > Billing Settings > Invoice Settings - Default Options' section.

- You can also approve the Invoice without adding payment and then use the 'Add Payment' option.
Add Procedure Code to Multiple Invoices
If you need to add a set of Procedure Codes to multiple Invoices, follow the steps given below.
- Go to 'Billing > Invoices'
- Select the Invoices for which you need to add the Procedure codes.
- Click the 'Actions' button above.

- Select the 'Add Procedures to Invoices' from the list.

- Enter the Procedure Code or Description.
- If you need to add the procedures to the Claim, enable the 'Add Procedures to Claim' option.
- Click the 'Add' button to add the Procedure Codes to the multiple Invoices.
Send Multiple Invoices to Patients
The Practice can send multiple Invoices to Patients by following the steps below.
- Go to 'Billing > Invoices'
- Select the Invoices to send and click the 'Send Invoices' button.

- Choose the delivery modes or set a preferred order for sending Invoices.
a. Send Through Selected Modes

- Choose one or more modes (PHR, Email, or Cell Number) to send Invoices.
- The Invoices will be sent only through the selected modes.
- If a Patient does not have the selected mode, the Invoice will not be sent to the patient.
- Example: If only PHR and Email are selected, and the Patient has only a Cell Number, they will not receive the Invoice.
b. Send Based on Preferred Order

- Arrange the preferred modes in priority order (e.g., PHR > Email > Text Message (Cell Number)).
- The Invoices will be sent through the available mode(s) based on the order.
- You can choose to send Invoices through:
- Only the first available mode (e.g., If a Patient has both PHR and Email, the Invoice will only be sent via PHR).
- The first two available modes (e.g., If a Patient has both PHR and Email, the Invoice will be sent through both).
Note: To set the default delivery preferences, go to 'Settings > Billing > Billing Settings > Sending Invoices - Defaults'.
Invoices Sent History
- The Invoices sent get listed under the 'Billing > Invoices > Invoices Sent History' section.

- This section lists the Invoice Sent Date, Sent Mode, Total number of Invoices sent, and number of Invoices sent successfully.
- You can also check the 'Invoice Sent' details under the 'Messages > Sent' section.
Claim Generation
Generate Claim(CMS1500)
The Practice can generate the Claim from an Invoice in order to submit it to the Payer.
- Go to 'Billing > Invoices'
- Click the 'More Options' (...) icon against the Invoice and select the 'Generate Claim (CMS1500)' option.


- The Patient Insurance details get auto-populated from the Invoice or Patient details. You can edit the Insurance details by clicking the 'Edit' icon next to the Insured name.
- Click the 'Save' button to generate the Claim. The generated Claims get listed under the 'Billing > Claims' section.
Edit Claim (CMS1500)
The generated Claims can be edited by following the steps given below.
- Go to 'Billing > Invoices' or 'Billing > Claims'
- Click the 'More Options' (...) icon against the Invoice or Claim and select the 'Edit Claim (CMS1500)' option.

- Make the required changes by clicking the 'Edit' icon against the respective fields and then click the 'Save' button.
Bulk Actions on Invoices
The following actions can be done by selecting multiple Invoices from the 'Billing > Invoices' section.

Add Notes
To add Notes to multiple Invoices, follow the steps given below.
- Select the Invoices you need to add Notes.
- Click the 'Add Notes' option under the 'Actions' button.

- Enter the notes and click the 'Add Notes' button.
Add Follow-up date on Multiple Invoices
- Practices can also set the follow-up date for multiple Invoices simultaneously.
- Select the Invoices and click the 'Set Invoice Follow-up' option under the 'Actions' button.

- Practices can filter out the Invoices that are due for follow-up by selecting the 'Search Option 1 > Invoices for Follow-up'
- The first option - Invoices for Follow-up - Allows Practices to view the Invoices that are due for follow-up.
- The second option - 'Upcoming Invoices for Follow-up' - Shows Invoices that need follow-up in the future.
- The third option - 'Invoices followed up' - Shows Invoices that are already followed up.

Flag/Un-flag the Invoices
You can flag/un-flag multiple Invoices at once by following the steps given below.
- Select the Invoices to be flagged.
- Click the 'Flag Invoices' option under the 'Actions' button. The Invoices get flagged.

- To un-flag the Invoices, select the Invoices and click the 'Clear Flags' option under the 'Actions' button.
Mark As Mailed
The physical copies of multiple Invoices sent to the Patients can be 'Marked as Mailed' by the Practice.
- Select the Invoices to be marked as mailed.
- Click the 'Mark As Mailed' option under the 'Actions' button.

- Select the Mailed Date and Mailed By options. The address of the respective Patients will be taken as Mailed Address. Enter the Comments, if any.
- Click the 'Mark As Mailed' button.
Mark/Unmark Invoices to 'Sent for Collection Agency'
The Practice can mark all the Invoices that are forwarded to Collection Agency at once, by following the steps given below.
- Select the Invoices to be marked as Sent for Collection.
- Click the 'Mark Invoice(s) as 'Sent for Collection'' option under the 'Actions' button.
- To clear the Invoices marked as Sent for Collection, select the 'Clear 'Sent for Collection'' option.
Delete the Draft Invoice
All Draft Invoices can be deleted in a single click by following the steps given below.
- Go to 'Billing > Invoices'
- Select the draft Invoices to be deleted.
- Click the 'Delete Draft Invoices' option under the 'Actions' button.

Bulk Edit Invoices
Practices can edit more than one Invoice simultaneously from the 'Invoices' section, making it easier to apply changes across multiple records.
- Navigate to 'Billing > Invoices' and select the Invoices to edit.
- Under the 'Actions' button, select the 'Edit Invoices' option.
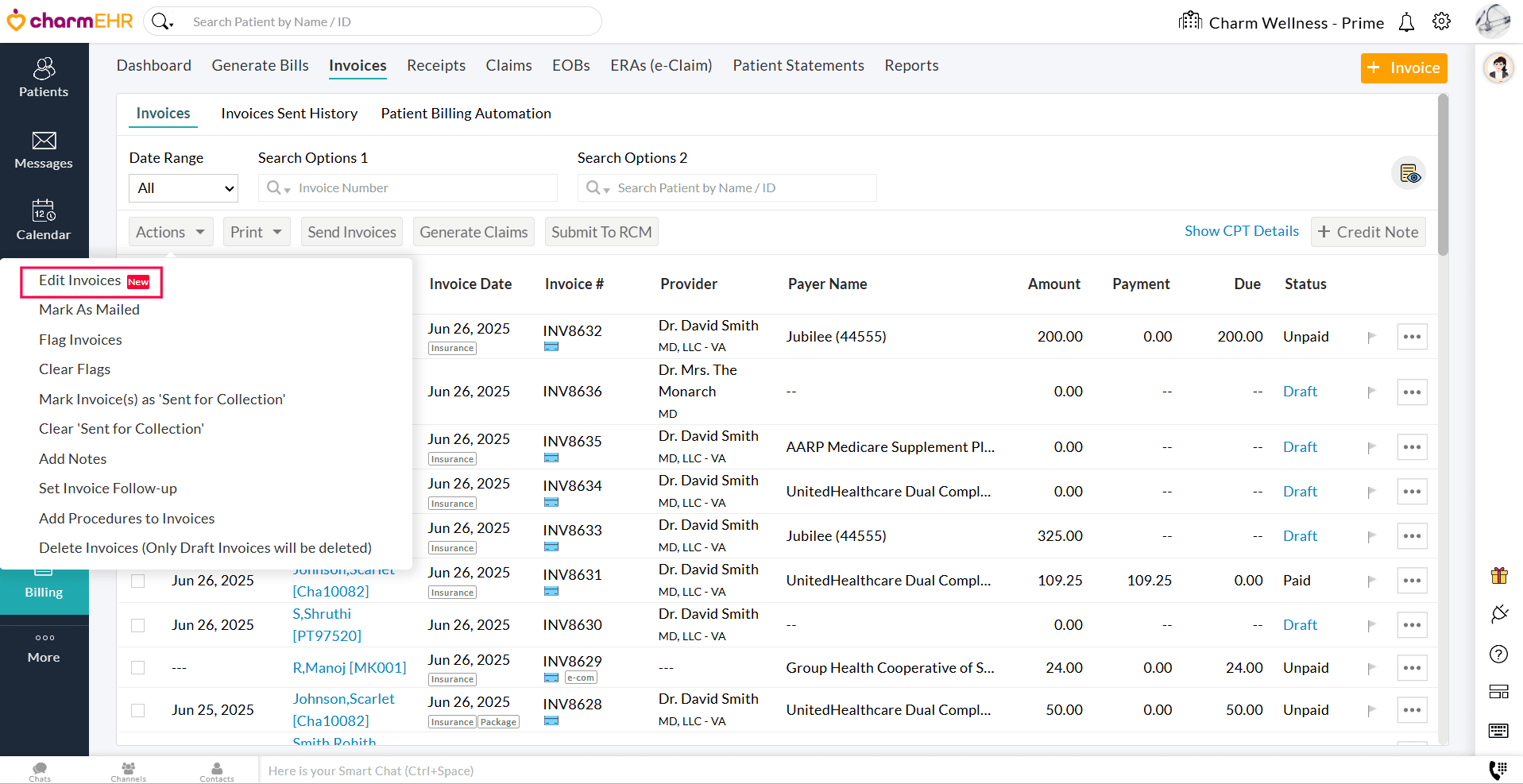
- Make the necessary changes and approve the Invoices.
Handling Credit Notes
An Invoice is created for the services rendered and products dispensed. If the Patient cancels any services or returns the products either partially or fully, the Practice can generate a 'Credit Note' for the Invoice. Creating Credit Note helps the Practice to have proper bookkeeping. Once products are refunded, the refunded quantities will be adjusted automatically in the Inventory.
Create Credit Note
To create a Credit Note for an Invoice, follow the steps given below.
- Navigate to 'Billing > Invoices'
- Click the 'More Options' (...) icon against the Invoice to create a Credit Note.
- Select the 'Return Items/Credit Note' option.
Note: This option is available for Invoices with 'Unpaid', 'Partially Paid', 'Paid' status.

- The Procedures/Products of the Invoice get listed. Keep the items that the Patient is returning. Edit the Returned Quantity under the Products section, if required.
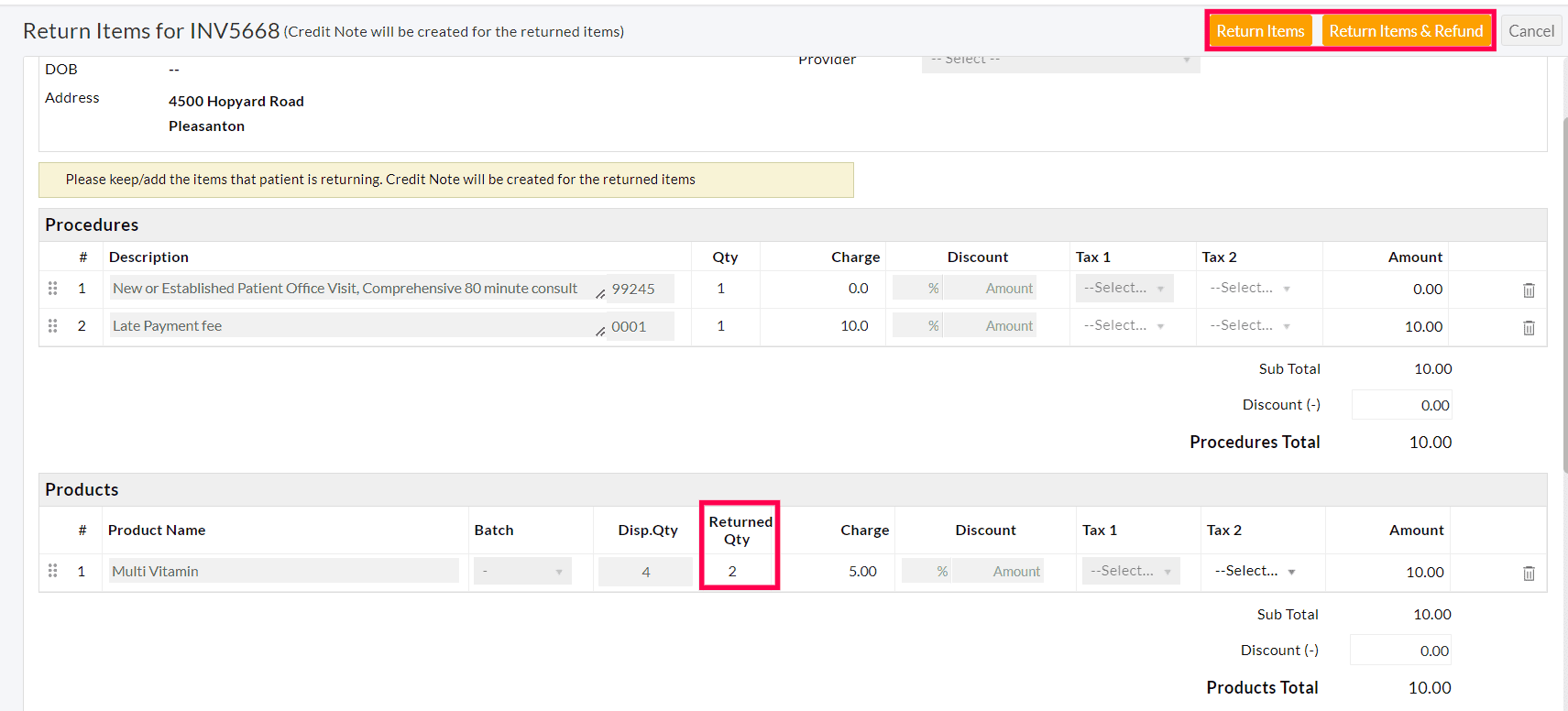
- Click the 'Return Items' or 'Return Items & Refund' button.
Return Items
- When the Invoice has no payments, use this option to collect items from the Patient without Payment Refunds.
- It creates a Credit note and the available quantity of the products will be adjusted in Inventory.
Return Items & Refund Payment to Patient
- This option is applicable only if the payments are added to the Invoice.
- It creates a Credit note and the available quantity of the products will be adjusted in Inventory.
- Also, the Payment Refund gets added to the Invoice Payment Receipts.
- Click on the 'Payment Refund' button to give a refund for the Patient.
- Click on the 'Cancel' to have it as an Unused Amount and use it for other Invoices.

Apply Credit Note
The Credit Note amount can be applied to the outstanding Invoices of the Patient by following the steps given below.
- Go to 'Billing > Invoices'
- Click the 'More Options' (...) icon against the Credit Note created.
- Select the 'Apply Credit Note' option.

- The outstanding Invoices of the Patient get listed.
- Apply the Credit Note amount to the outstanding Invoice(s). The payment applied amount should not exceed the Invoice due.
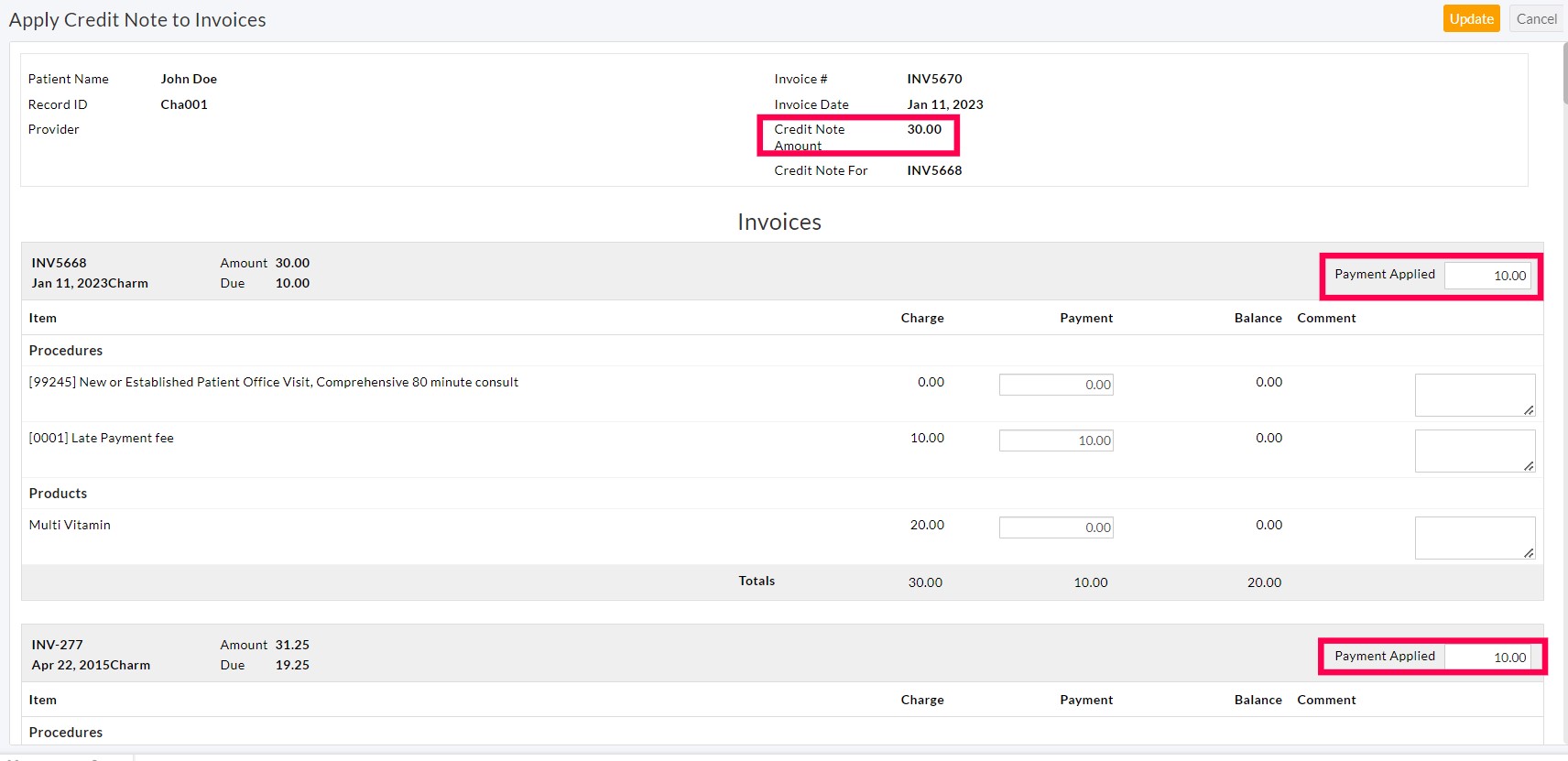
- The Credit Note amount gets applied to the outstanding Invoices.
Credit Note Status
All Credit Notes are categorized under 2 statuses, i.e 'Open' and 'Closed'.
- 'Open' status: Unpaid and Partially Paid Credit notes are shown as 'Open'.
- 'Closed' status: Paid Credit notes are shown as 'Closed'.
Delete Credit Note
A Credit Note can be deleted only if it is 'Not Applied' to any Invoice. If applied, follow the steps given below to delete the Credit Note.
- Select the 'Apply Credit Note' option of the Credit Note to be deleted.
- For all the applied invoices, clear the 'Payment Applied' field and click on 'Update'.
- Delete the Credit Note by clicking the 'Delete' option under the 'More Options' (...) icon.
- The Product quantities will be deducted from the Inventory after deleting the Credit Note.

Handling Refunds
- While generating a Credit Note, the Products can be returned to the Inventory and the payment amount can be refunded in a single place under the 'Billing > Invoices' section.
- On creating a Credit Note, click the 'Return Items & Refund' button at the top right corner.
- This option reverts/revises the payments posted for the Invoice and opens the 'Payment Refund' dialog to initiate refunds.
- The Payment Refund gets added to the Invoice Payment Receipts.
- Click on the 'Payment Refund' button to give a refund for the Patient.
- If the Payment is made through Bluefin Payment Gateway, two options will be available.
- Refund through Payment Gateway: On selecting this option, the refund will be given to the Patient's card through the Payment Gateway, and the Refund entry will be added to the CharmHealth.
- Refund given in Payment Gateway Console. Add refund entry in CharmHealth: This option can be selected when the Refund is made in the Payment Gateway Console. Only the Refund entry gets recorded in CharmHealth and no actual Refund will be given to the Patient's Card.

Invoices - Watchlist
Invoices Watchlist helps the Practice to view the important data in consolidation. The Practice Members can click the separate items to get finer details and take action accordingly.

- Click the 'Watchlist' icon in the top right corner of the 'Billing > Invoices' section. The following items get displayed.
- Draft Invoices: This shows the total number of Invoices in the 'Draft' status. The Practice can work on these Invoices later.
- Invoices with Due & PR: Shows the total number of Invoices with 'Due and Patient Responsibility'. The Practice can work on these Invoices to close them by applying for the unused payments if available for the Patient or can follow up with a Patient by sending the Invoices/Statements for payments.
- Invoices with '-ve' Due: The Practice can use this to identify the Invoices applied with additional payment/ adjustment. These can be invoices with additional payments from EOBs or when a paid invoice is edited and items are removed, it can be an invoice with a '-ve' balance.
Usage of 'Date Range'
This filter lists the Invoices based on the selected Date Range. By default, all Invoices in your system get listed. You can select one of the pre-configured filters, as shown in the screenshot below, or enter your own custom date range for the filter.

Using 'Search Options 1' and 'Search Options 2'
Search Options 1:
Invoices of the Patients get listed based on the search options available, as shown in the screenshot below.

- Invoice Number: Enter the Invoice number for a quick search.
- Invoice Status: Patients get listed based on the Invoice Status Viz., Paid, Unpaid, Partially paid, Unpaid or Partially Paid, Draft, Canceled, and Negative Due (Due<0).
- Invoice Type: Opt to list the Invoices or Credit Notes.
- Provider: List the Invoices based on the selected 'Invoice Provider'.
- Payer Name or ID: Enter the Payer Name or ID to list the Invoices generated for a particular Payer.
- Insurance Plan Name: Enter the Insurance Plan name to list the Invoices of a particular Insurance plan.
- Outstanding Invoices: List all the outstanding Invoices in the selected date range. Choose the required option from the drop-down menu, as shown in the screenshot below.

- Outstanding for N Days: List the Invoices that are outstanding for N number of days, viz., 10 days, 20 days, 30 days, 60 days, 11 to 20 days, 21 to 30 days, etc. The Practices can view two groups of search options: one to filter Invoices based on the Invoice date and the other to filter Invoices based on the first Invoice sent date.

- Procedure Code: List all the Invoices with a specific Procedure Code.
- Has Claim: List the Invoices that have a Claim. To refine your search, choose the required option from the drop-down menu, as shown in the screenshot below.

- Has Notes: Invoices with or without Notes get listed.
- Has Encounter: Select this option to list the Invoices with Singed Encounter, Un-signed Encounter, or no Encounter.
- Is Invoice Sent: List the Invoices sent to the Patients through PHR, EMail, Cell Number, and Mail. You can also choose to list the Invoices that are not sent to the Patients.
- Is Invoice Flagged: Select this option to list the Flagged or Un-flagged Invoices.
- Is Invoice Sent for Collection: Select this option to list the Invoices sent to the collection agency.
- E-Commerce: Invoices generated for E-Commerce orders from Inventory can be viewed by selecting this option.
- Is Submitted to RCM: List the Invoices submitted to RCM. Choose the required option from the drop-down menu, as shown in the screenshot below.

- RCM Claim Options: Filter the Invoices based on the RCM Claim options viz., Has No PR, Has PR, Has Due and Secondary Exists, Has PR & Invoice Due, and Has PR, Due & Not sent to Patient.
- Patient Billing: Practices can filter Invoices sent 30 days prior and can send the first reminder to Patients. Additional options to filter Invoices by 60 days, 90 days, etc., are also provided.
- Patient Has Card on File: The Patients with Card on File gets listed. You can further refine your search by using the following options viz., Invoice with Due, Invoice with Due & PR, Invoice with Due & Patient has no Card on File, and Invoice with Due, PR & Patient has no Card on File.
- Patient Communication: The Patient's name get listed based on the mode of communication viz., Patients with PHR, Email, Cell Number, Email but no PHR, and Cell Number but no Email.
- Recurring Payments: You can filter Invoices with Patients having recurring payments. It helps the Practices to exclude those invoices & charge the remaining Invoices as part of the Patient billing.
- Patient's Age on or above: Lists all the Patients who are a certain age or older.
- Patient's Age Below: Lists the Patients under a certain age in years.
Search Options 2
The additional search option allows applying two filters at the same time to speed up your process. You can use the option 'Search Options 2' provided under the 'Invoices List View' section to filter their Invoices based on your needs.

Sorting option on 'Invoices List View'
Use the Sort Order menu to change the order of rows on the 'Invoice List View' page. To change the order of the columns, hover the mouse pointer over the area to the right of the column name in the header and click either the upward-facing triangle (Sort Ascending) or the downward-facing triangle (Sort Descending) for that column.
- Encounter Date: You can sort the Encounter Date from Oldest to Newest or from Newest to Oldest.
- Patient Name: Sort the Patient's Name in alphabetical order of First Name.
- Invoice Date: You can sort the Invoice Date from Oldest to Newest or from Newest to Oldest.
- Invoice#: Sort the Invoice# in ascending or descending order.
- Provider: Sort the Provider's Name in alphabetical order of First Name.
- Payer Name: Sort the name of the Payer in alphabetical order.
- Amount: You can sort the Amount from low to high or vice versa.
- Payment: Sort the Payment amount from lowest to highest or vice versa.
- Due: Sort the payment due amount from lowest to highest or vice versa.
- Status: You can sort the Invoice by its Status in alphabetically.
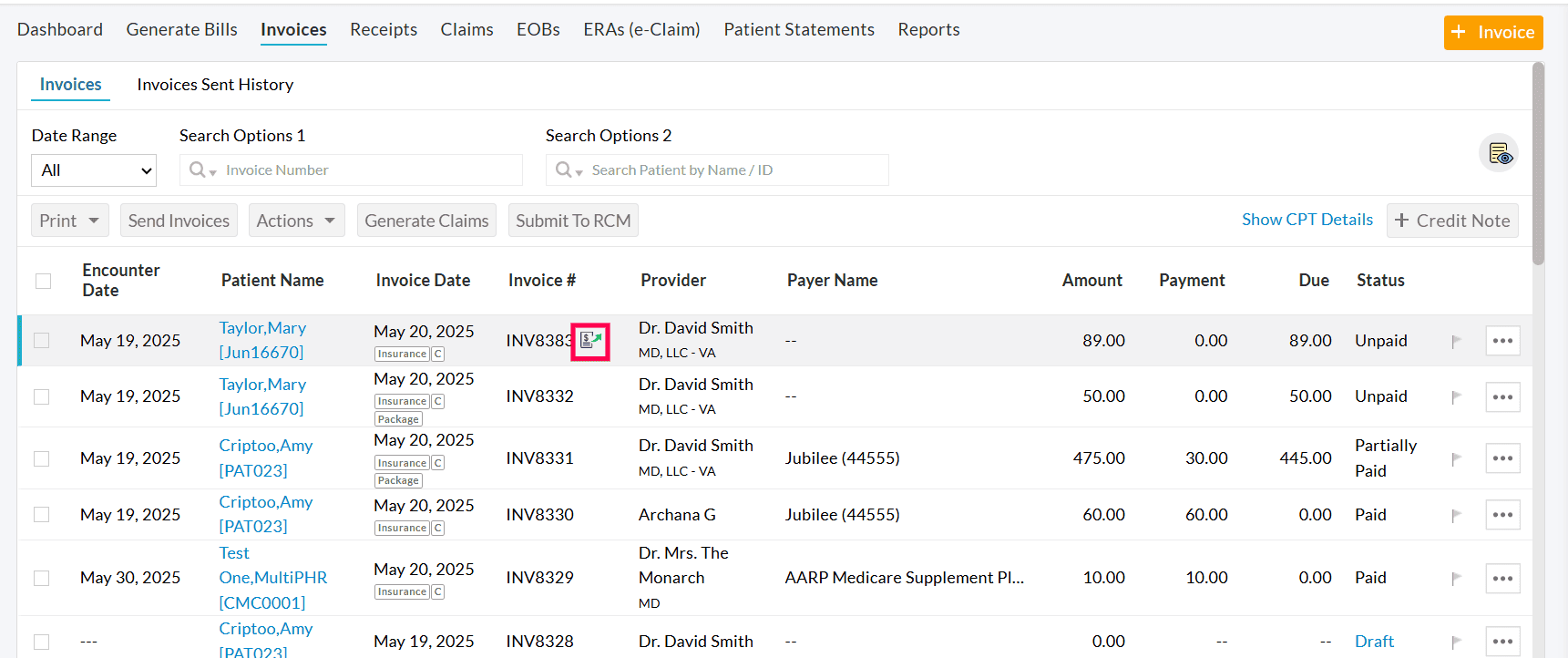
Details of Icons (Insurance/C/Card/Credit Note/etc.) shown in 'Invoices List View'
The icons give quick details about the Invoice in the 'Invoice List View'. The following icons are available.
- Insurance: Insurance selected while generating the Invoice. This indicates that the Practice wants to generate Claims for Invoices with Insurance.
- C: Claim generated for the Invoice.
- Card: Indicates that the 'Card on File' is available for the Patient.
- Credit Note: Indicates that it is a 'Credit Note' generated for returning services/products back to the Patient.
- Notes: Invoices with Notes.
- RCM: Invoices submitted to RCM.
- Mail icon: Invoices sent to the Patients.
- Package: Package sold in the Invoice.
- Card icon: Patients with saved Card(s) on File.
- Icon for Invoice Sent For Collection

For Practices Working with CharmRCM or CharmBillerPro
The Practice with the CharmRCM Services enabled, can do the following actions in the 'Invoices' section.
- Submit to RCM
- Submit to RCM with Notes/Attachments
- Multiple Invoices - Submit to RCM
- Search Options
Submit to RCM
Once the Invoice is generated, the Providers can choose to submit the Invoice to collect money from the Insurance Company.
- Navigate to Billing > Invoices
- Select the Invoice and click the 'More Options' (...) icon.
- Select the 'Submit to RCM' option.
- The submitted Invoice gets labeled with the 'RCM' tag.

Note: If there is any missing information required for Claim generation, an error appears with the details of missing items as shown in the screenshot below.

Update the Encounter and submit it to RCM. The mandatory information can be configured in your BillerPro account. Go to the 'Admin Settings > Mandatory Chart Details from Practice' section and select the mandatory information required while submitting the Chart to RCM.
Submit to RCM with Notes/Attachments
- To submit the Invoice with notes/attachments, select the 'Submit to RCM with Notes/Attachments' option under the 'More Options' (...) icon against the Invoice.

- Enter the additional information for Claim processing and attach the files related to the Encounter.
- Click the 'Submit to RCM' button.
Multiple Invoices - Submit to RCM
If you need to submit more than one Invoice to RCM, select the Invoices and click the 'Submit to RCM' button above.

Search Options
- Is Submitted to RCM: To list the Invoices submitted to RCM, select the 'Is Submitted to RCM' option from the 'Search Options 1'. Choose the required option from the drop-down menu, as shown in the screenshot below.

- RCM Claim Options: Filter the Invoices based on the RCM Claim options viz., Has No PR, Has PR, Has Due and Secondary Exists, Has PR & Invoice Due, and Has PR, Due & Not sent to Patient.

Invoice - Reports
The Invoice Report gives a detailed overview of all Invoices created in a given period. You can customize it to show a particular range of Invoices with the filters. Go to the 'Billing > Report' section to view the following reports.
Invoices List
- This report lists the Invoices generated in the selected Date Range.
- You can group the report by Facility Name, Facility Code, Patient Name, Provider, Payer Name, Generated/Updated by, Facility Resource, Invoice Type, Referral Source, Referral Specific Source, Invoices With Encounter, and Invoice is Sent for Collection.
- The report gets listed according to the selected parameter in the 'Group by' option.
- You can also search the Invoices using the Filter options and generate the report.

- Click the 'Show Report' button to view the Invoice Report grouped by the selected parameter.
- You can export the report as a CSV file by clicking the 'Export as CSV' button. Enable the 'Export all the report details with subtotals' option to export all details with subtotals. Else, only the subtotals will get exported.

- To export only the particular columns in the report as a CSV or PDF file. Click the 'Settings' icon next to the 'Export Selected Columns' button and drag and drop the column names from the Available Columns to the Selected Columns. Choose the PDF Layout either as a Landscape or a Portrait, and click the 'Update' button.

- To save the report as a Custom Report, click the 'Save as Custom Report' button. Enter the Report Name, Description, and choose the Category. To add a new Category, click the 'Add New' link.

Invoices by Patient
- Go to 'Billing > Reports > Invoice Reports > Invoices by Patient'
- This report lists the Invoices grouped by Patients' name.
- Choose to show the Invoices either by Invoice Date or Encounter Date and select the Date Range.
- Click the 'Show Report' button to generate the report.

- This report can be downloaded as a CSV file by clicking the 'Export as CSV' button.
Invoices by Provider
- Go to 'Billing > Reports > Invoice Reports > Invoices by Provider'
- This report lists the Invoices grouped by Provider.
- Choose to show the Invoices either by Invoice Date or Encounter Date and select the Date Range.
- Click the 'Show Report' button to generate the report.

Invoices List for Collection Agency Report
- Go to 'Billing > Reports > Invoice Reports > Invoices List for Collection Agency Report'
- This report lists the Invoices sent to the Collection Agency.
- Choose to show the Invoices either by Invoice Date or Encounter Date and select the Date Range.
- Practice can use this report to export patient and guarantor details that can be sent to the collection agency.
- To view all the invoices including the ones marked as 'Sent for Collection' invoices, Practice can use the combination of 'Show Details by --> Invoice Date' & 'Fetch All Invoices' filters.
- Click the 'Show Report' button to generate the report.

Preferred Settings for Cash-based Practices
For Practices that support Patients directly without getting involved with insurance companies, the following settings can be configured.
- Choose 'Pay Invoice in Full' as the default auto-payment option while generating an Invoice and as well as while adding payments under the 'Settings > Billing > Billing Settings > Invoice Settings - Default Options' section.
- Choose 'Yes' for the 'Auto-apply 'Adjust the available patient credits against the invoice' while invoicing' option under the 'Settings > Billing > Billing Settings > Invoice Settings - General' section.
Preferred settings for Cashless Practices (Insurance based)
The following settings can be configured by the Practices that deal with the Insurance companies in providing claim payments.
- Choose the default auto-payment options while generating an Invoice and as well as while adding payments under the 'Settings > Billing > Billing Settings > Invoice Settings - Default Options' section. For Cashless Practices, enable the 'Pay Products in full, Pay Copay, & Pay Non-Covered Services'.
- Choose 'Yes' for the 'Enable item level payments for Invoice' option under the 'Settings > Billing > Billing Settings > Invoice Settings - General' section.
- Choose 'Yes' for the 'Auto-select 'Primary Insurance' of patient in Invoice' option under the 'Settings > Billing > Billing Settings > Invoice Settings- General' section.
- New Payer can be added using the '+ Payer' button available in the 'Settings > Billing-Claims > Payers' section.
- When the Practice works with a pre-configured list of Payers, the 'We work with a pre-configured list of payers and we accept patient insurances only with these payers. We do not want patients or practice members to add new payer or payer address details' option should be enabled under the 'Settings > Billing-Claims > Payers' section. If this option is enabled, all the verified Payers in this list will be available for the Patients/Practice members for selection while adding the Patient Insurance details.
- Patient Insurance can be added using the '+ Insurance' button under the 'Patient > Patient Details > Insurance' section.
Hard Closing of Accounts
'Hard Close' is a feature introduced for the effective accounting of Billing entries. This feature will be useful for the Practices that take billing information from CharmHealth to accounting software for accounting or for taxation purposes. When you enable this feature, you will find a new option 'Hard Close' in the 'Billing > Invoices' tab, where the option to hard close data up to a specific date will be available. Generally, Practice will choose the last date of the month as the date for hard closing.
When the 'Hard Close' option is used, all entries - 'Invoices, Receipts, & Refunds' within the selected date will be hard closed. At the time of editing/modification of these hard-closed entries, a warning message will be shown that these entries are already hard-closed, and the user can still modify them. All the entries modified after the hard closing will be available in 'Hard Close - Modified Entities Report' shown under the 'Billing > Reports > Other Reports' section. One can check this report to verify the changes made after the hard closing and make necessary changes to the entries in the accounting.
