Claims
- Claim Generation
- Claim Settings
- Automatic claim generation and claim settings
- Claim Validation
- Claim Submission
- Billing for the Products/Drugs
- Adding Claim Payments
- Managing Claim Denials
- Handling Claim Rejections and Claim Resubmission
- Edit and Preview Claims
- Claim Versioning
- Resending Corrected Claims and Appeals
- Claim Follow-up
- Usage of 'Date Range'
- Claim Search Options
- Additional Search Option
- Claim Actions and Bulk Actions
- Handling Secondary Claims
- Handling Billing when provider leaves the Practice
- Default ID Qualifier for Billing
- Claims - Watchlist
- Claims - Reports
Claim Generation
Generate Claim
When Practices want to bill the Payers (Insurance Companies) for the Services/Procedures rendered to the Patient, they can generate Claim for the Invoice and submit it to the Payers. To generate a Claim, follow the steps given below.
- Navigate to 'Billing > Invoices'
- Click the 'More Options' (...) icon against the Invoice and select the 'Generate Claim (CMS1500)' option.

- All required details get auto-populated by the system based on your Claim settings. You can verify these details and click the 'Save' button to save the details.
Bulk Claim Generation
Multiple Claims can be generated in a single click by selecting the Invoices and clicking the 'Generate Claims' button.

Once the claims get generated, a preview of the Claims is shown. If there are any warnings/errors, it is indicated by a warning sign beside the Claim. You can navigate to the Claim and edit as required.


Adding Dx and Reordering Dx in Claims
Diagnosis Codes can be added and reordered only if the settings under 'Settings > Billing-Claim Settings > Diagnosis Settings' are enabled. To know more about the Diagnosis Settings, click here.
You can add Dx Codes while generating the Claim by clicking the '+' icon in the Box#21.

You can reorder Diagnosis Codes using drag/drop based on the priority. Changes done in this section will be reflected automatically to the Encounter.
Add Procedures to Claim
To add Procedures to a Claim, follow the steps given below.
- Navigate to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Edit Claim (CMS1500)' option.
- In Box#24, click the '+' icon and add the Procedures to the Claim.

- Click the 'Save' button to update the changes.
Automatic claim generation and claim settings
CharmHealth has a feature to generate claims automatically as and when an invoice for an Encounter gets approved. This saves the user time in generating the claims manually. The user can configure the necessary settings for claim generation as explained in the 'Claim Generation Settings' section.

Claim Validation
This feature does an automatic validation of Claims to detect errors and warnings. For Practices with Optum Clearinghouse, the Claims are automatically sent to Optum for ACE Testing. The Claim validation is done for both manual and bulk Claim generation, as well as for the automatically generated Claims.
The Claims are categorised into three groups - Clean Claims, Error Claims, and Warning Claims.
Settings to Enable/Disable Automatic Optum ACE Testing
Practice Members have the option to enable or disable the automatic ACE Testing in Charm that will automatically submit to Optum when a Claim is generated or modified.

Filter Clean Claims and Claims with Errors/Warnings/ACE
Claims are categorised into three groups: Clean Claims, Error Claims, and Warning Claims. The Billers can view the corresponding icons of each category in the Claim list view, located below the status. Detailed information about any errors or warnings can be accessed by previewing the Claim or editing the Claim in the CMS1500 format.
 |
Claim Errors |
 |
Claim Warnings |
 |
ACE Errors from Optum |
 |
ACE Warnings from Optum |
The Practice Members can use the 'Has Warnings/Errors' option to filter the Clean Claims, Error Claims, or Warning Claims. Once the Claim gets submitted, these error/warning icons against the Claim will not be shown.


The Practice Members can also filter the Clean Claims in the e-Claim submission page (Claims > e-Claim Submission) and submit them.

You can also view the overall count of Claims that have errors, warnings, or ACE under the Claims watchlist.

More detailed information about any errors or warnings can be accessed by previewing the Claim or editing it in the CMS1500 format.


Claim Submission
On generating, the Claims are submitted to the Payers either electronically or through Fax or Paper Mail. All claims generated get listed under the 'Billing > Claims' section.
Electronic Claim Submission
For the Practice subscribed to the E-Claims add-on, the Claims can be electronically submitted from CharmHealth to the payers. Upon successful submission, the status of the Claims will be automatically changed to 'Submitted Electronically'.
To know more about the process of Electronic Claim Submission, click here.
Print Image File (PIF) - Batch Claim PIF
Practices can download the Batch Claim PIF using the two options below.
Download Claim PIF of 'Not Submitted' Claims
Practices can download the Claim PIF for Claims with the statuses 'Not Submitted' or 'Ready for Resubmission'.
- Navigate to 'Billing > Claims'
- Click the 'Batch Claim PIF' button.

- Select one or more Claims and click the 'Download Batch Claim PIF' button.
- Practices can update the Claim status to 'Submitted to Payer' on downloading the Claim PIF using the 'Download Claim PIF & Update Status' button.

Download Claim PIF of Selected Claims
Practices can download the Batch Claim PIF files for selected Claims, including previously submitted Claims.
- Go to 'Billing > Claims'.
- Use the Search Options to filter the Claims list by Payer, Claim Status, etc.
- Select one or more Claims from the list.
- Click the 'Action' button and select 'Download Batch Claim PIF'.

The selected files are downloaded in Plain text (.TXT) format.
Printing claims on CMS1500 form
If you need to send Claims through Paper Mail, use the 'Print Data on Claim' option to download the Claims.
Print Claim Data On CMS1500 Form - option
To generate a PDF file for printing in the CMS1500 form, follow the steps given below.
- Navigate to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Print Data on Claim CMS1500 Form' option.
- A PDF file gets downloaded to your system.
CMS1500 Print Settings
The Practice can configure the CMS1500 Print Settings under the 'Settings > Billing-Claims > CMS1500 Print Settings' section.
- Printing Claim Total Charge in CMS1500 Form when more than six line items are in a Claim: When there are more than six CPT codes in a Claim, each page of the printed claim will have up to six line items, and the total claim amount will be printed on each page by default. As requested by a few Payers, the total claim amount gets printed on the last page of the Claim on choosing the second option of this setting. For example, if there are 10 line items in a Claim, the first CMS page will have six line items, and the second page will have four line items. Using this setting, the Claim total charge of all the 10 line items can be printed on the second page of the CMS1500 form.
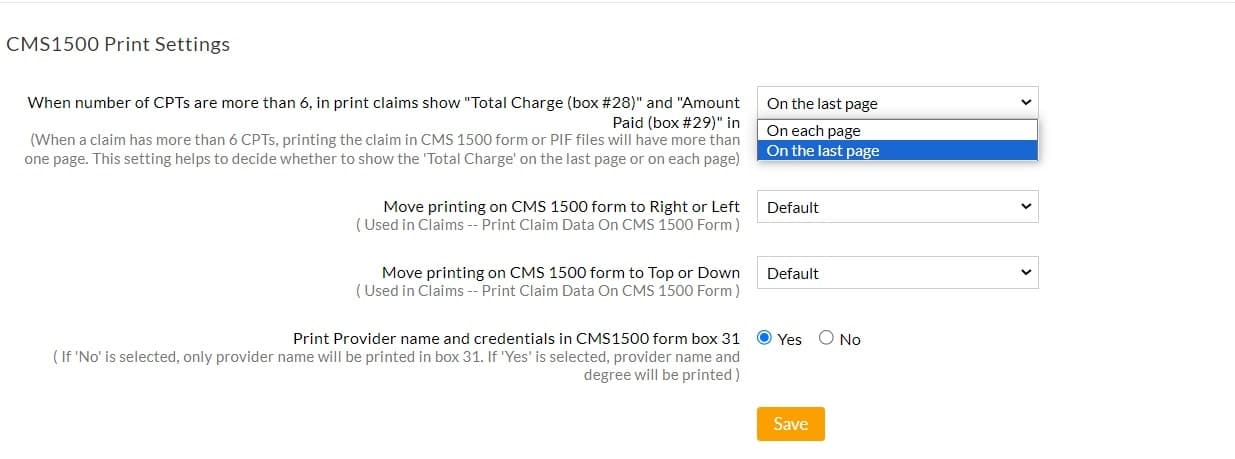
- Shift the printing on the CMS 1500 form to either left or right.
- Shift the printing on the CMS 1500 form to either top or bottom.
- To print the Provider name and credentials in Box# 31, the Practice can enable the 'Print Provider name and credentials in CMS1500 form box' option. If 'No' is selected, only the Provider name will be printed.
Faxing Claims
Claim with filled-in CMS1500 form, Encounter Summary, and other documents such as covering letter, EOB, etc., can be sent to the Payer in the desired order. This option will be available to Practices for which the 'Fax Service' is enabled.
- Navigate to 'Billing > Claims'
- Click the 'More Options' (...) icon against a Claim and select the 'Fax Claim' option.
- Sent and Received Fax details will be shown in the dialog.
- Click the 'New Fax' link to send a new Fax to the Payer.

- Enter the details such as 'Fax Number', 'Recipient Name', etc., and select the required attachments. You can include the Medical Records with the Claim and send them to the Payers.
- Use the 'Drag and Drop' option to re-arrange the attachments.
- Click the 'Preview' button to preview the fax document.

- Click the 'Send' button to send the fax.
Note: Attachments are to be added using the 'Add/View Attachments' option of the Claim.
Mapping Received Fax to Claim
This feature helps to map a fax received to one or more Claims. This option is used mostly, when EOB or any communication from the Payer is received specifically to Claim(s). After mapping, the fax copy of the Claim(s) can be accessed from the 'Billing > Claims' section.
- Navigate to 'Messages' and click the 'Received' folder under the 'Fax' section.

- Select the required fax and click the 'Add to Claims' link.
- Search and select the Patient.
- Search and select the Invoices for which the fax needs to be mapped.

- Click the 'Add' button to map the fax.
- The mapped document will be shown under the 'Received Faxes' section of the 'Fax Claim' option of the Claim under the 'Billing > Claims' section.

Billing for the Products/Drugs
CharmHealth helps the Practices in streamlining the process of billing Products/Drugs. To enable billing for Products/Drugs, follow the steps given below.
- Navigate to 'Settings > Billing-Claims > Claim Settings'
- Choose the option 'Yes' for the setting 'Enable billing for Drugs', and click the 'Save' button.

Once this setting is enabled, the Practice members can add additional billing details to 'Drugs' in the 'Inventory' module. These additional billing details for drugs include 'CPT Code', 'NDC Code', 'NDC Unit of Measure', and 'NDC Unit Price'. The details added to drugs are used during the Claim generation of the drugs.
As a first step, an Invoice needs to be created with the necessary drug(s) prescribed/dispensed. When the Claim gets created from this Invoice, the respective 'CPT Code' configured for the drug will be added as a line item in the Claim CMS 1500 form. Additional drug details such as 'NDC Code', 'NDC Unit of Measure', and 'NDC Unit Price' are taken from the Inventory section and added in box# 24 shaded area automatically.
- Steps to configure NDC details while adding new Drugs in the 'Inventory' module
- Navigate to the 'Inventory' module.
- Click the '+ Inventory' option and select the 'Drug' option in the 'Group' field.
- Additional details for drug billing - 'CPT Code', 'NDC Code', 'NDC Unit of Measure', and 'NDC Unit Price' will be shown.

- When the 'NDC Code' is different for each stock of a drug, it can be added at the time of adding new stock.
- When the 'NDC Code' for a drug is the same for all the stocks, it can be added once when adding the drug for the first time.
- When the 'NDC Code' is added at the product level and the stock level, the details configured at the stock level will be used in the Claim.
- Steps to configure NDC details for existing Drugs in the 'Inventory' module
- Navigate to the 'Inventory' module.
- Click the 'More Option' (...) icon of the required Drug and click the 'Edit Product Details' option.
- Specify the 'CPT Code', 'NDC Code', and 'NDC Unit of Measure' details.

- Click the 'Update' button.
- The 'NDC Unit Price' can be configured using the 'Edit Stock Details' option.

- If the 'NDC Unit Price' is not configured, then 'Retail Price/Item' will be taken as 'NDC Unit Price' by default.
- Generating Claim with NDC Drugs
- Say, a drug 'Prozac 20 milligram(s) oral capsule' is dispensed, and an Invoice is created for this drug/product.
- When the Claim gets generated using the 'New Claim' option for this Invoice, the drug 'Prozac 20 milligram(s) oral capsule' dispensed in the Invoice will be added with the 'CPT Code' configured for the drug in the Inventory as a charge item along with the NDC details.
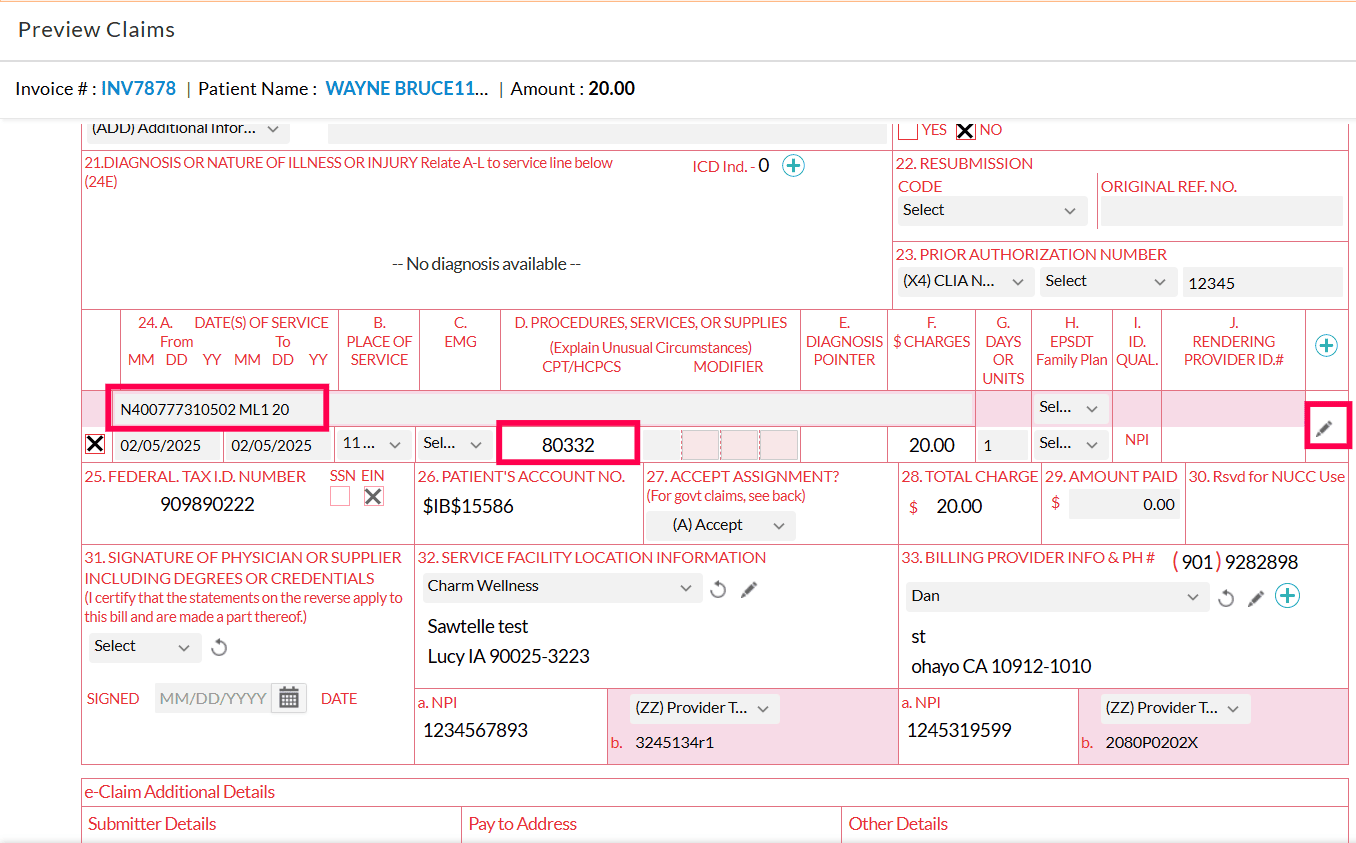
- The NDC details of the drug will be shown in the 'Comments (24)' field while generating the Claim. The sequence of NDC details are 'N4', 'NDC Code', 'NDC Unit of Measure', 'Quantity', and 'NDC Unit Price'.
- The details such as Diagnosis (Dx) Pointers, Modifiers, Place of Service (POS), etc., can be updated by using the 'Edit' icon of respective drugs.

- In the case of electronic claims, these details will be part of the electronic claim.
Adding Claim Payments
Automatic Payment Posting from ERAs
Electronic Remittance Advice (ERA) is an electronic form of claim payment information from the Payer with the Explanation of Benefits (EOB) details. On subscribing to the Electronic Claims add-on, you will receive ERAs electronically, and the payment gets posted automatically.
To know more about the ERA Payment Posting, visit the ERA & Payment Posting section.
Upload ERA
The Practice can manually download the ERAs ANSI 835 files from the Payer portal and upload them in CharmHealth using the 'Upload ERA' (ANSI 835) button under the 'Billing > ERAs' section. On uploading the ERA, CharmHealth will process and match the EOBs with the Invoices/Claims and post the payment automatically.
Add Payments from the EOBs section
If the Practice doesn't have the E-Claims add-on, they can post all the payments on an EOB received via Fax or Paper mail in the 'Billing > EOBs' section.
Click the '+EOB Details', and search and select the Patient's name or Record ID (or) Payer ID or Payer Name. This lists all the outstanding Invoices of the Patient. Click the 'Select' button to post payments for the respective Invoice/Claim.
To know more about the Payment posting of EOB, click here. (link from EOBs section)
Add Payment to a Claim
The payment can be added to a Claim individually by following the steps given below.
- Navigate to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Add Payment' option.
- Enter the Payment Amount and Payment Method.

- Click the 'Add' button to add the payment.
Managing Claim Denials
Adding Denials
While posting payments, if a CPT gets denied in an EOB, it can be marked as denied using the 'Denied' checkbox available at the right of the line item. On marking the CPT as denied, you can enter the denial code, type, and comment in the 'Comments' field.

Automatic Denials posting as part of ERA payment
During the automatic payment posting of ERA, the Denials get captured automatically by the system. This can be managed by configuring the setting under the 'Settings > Billing-eClaims > ERA Settings' section.

If the 'Apply values as given in EOB' option is selected, a payment amount of zero gets added to the CPT along with the adjustment gets posted to the Claim.
Claim Denials
The Claim Denials feature provides a centralized view to monitor, track, and manage all denied Claims from a single location. These insights help Practices streamline denial management, improve visibility, and take timely action to reduce repeat denials.
Using this feature, Practices can:
- Review denials grouped by category
- View a complete list of denied CPTs with descriptions and denial reason codes
- Track the Top 10 denial codes for the Practice
- Analyze Payer-wise denial trends
To access this feature, navigate to Billing > Claims > Claim Denials. The following filter options are available.
- Facility: View denials for a specific Facility or across all Facilities.
- Show Details by: Filter denials by:
- Claim Denied Date (Default)
- Claim Submission Date
- Encounter Date
- Claim Generated Date
- Claim Updated Date
- Date Range: View the denial list for the selected date range.
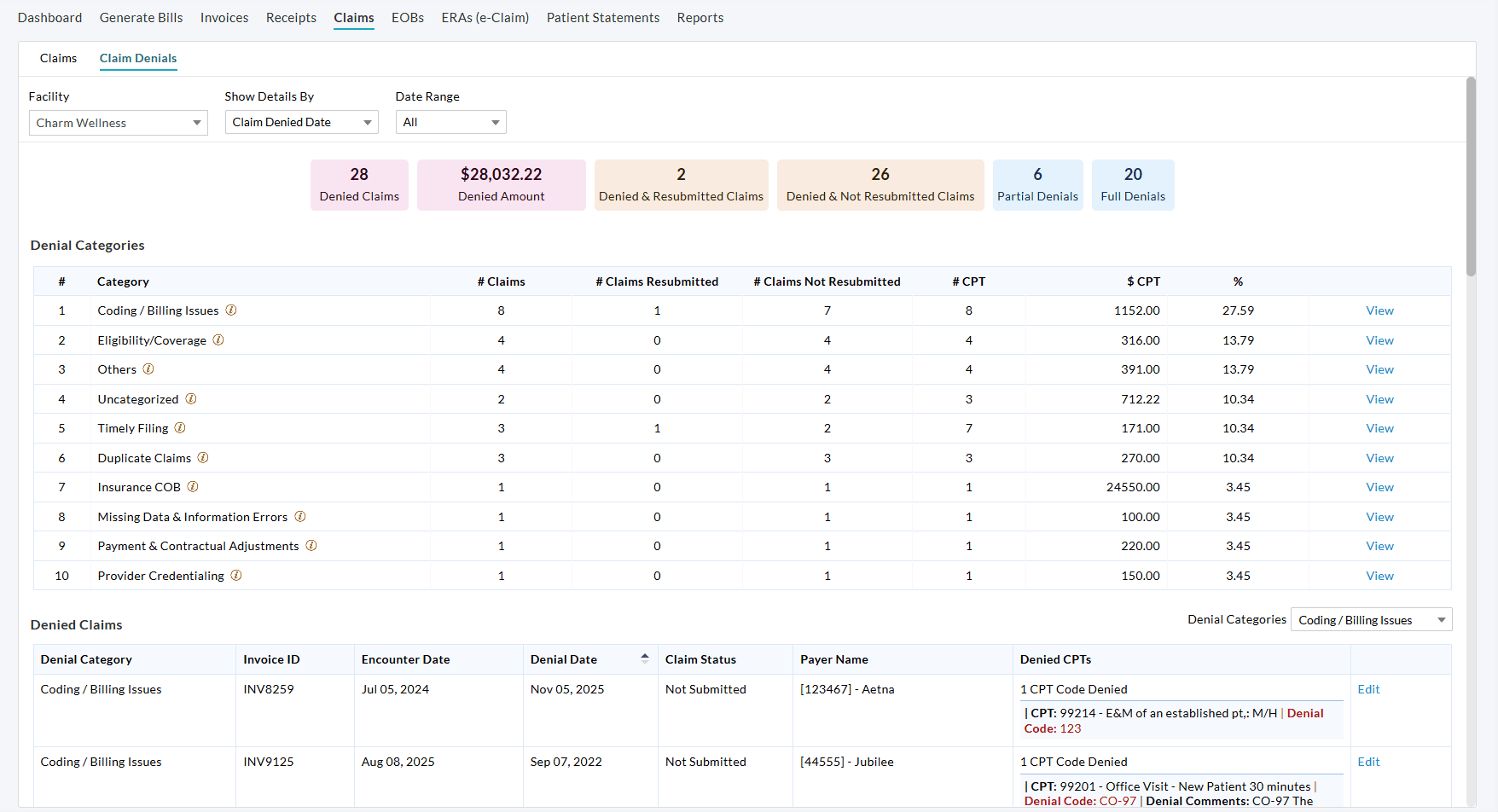
Denial Watchlist
The Denial Watchlist provides a quick summary of denial activity, including:
- Total number of denied Claims
- Total denied amount
- Number of denied and resubmitted Claims
- Number of denied but not resubmitted Claims
- Number of partially denied Claims
- Number of fully denied Claims
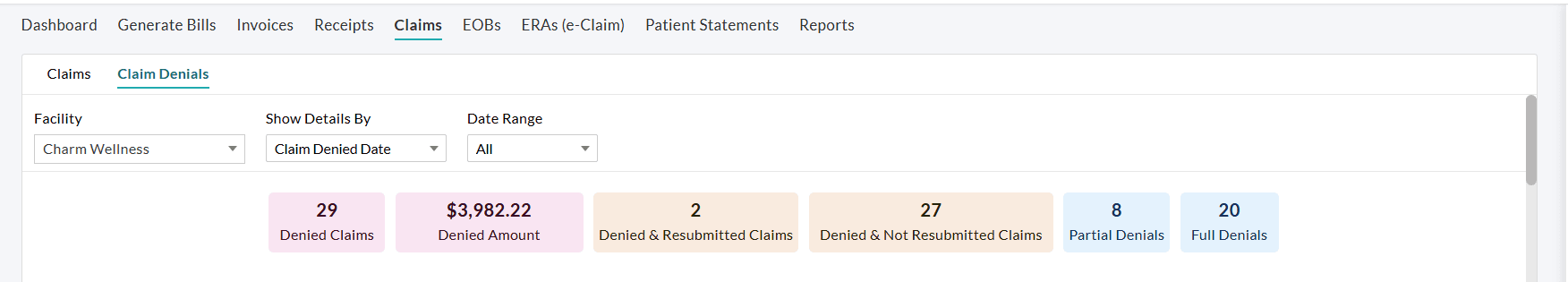
Click on any widget to access a detailed Claim list view of the corresponding denial activity.
Automatic Grouping of Denials by Denial Category
All denied Claims are automatically grouped by Denial Category for easier analysis. For each Category, you can view:
- Total number of denied Claims
- Number of resubmitted and not resubmitted Claims
- Number of denied CPTs
- Total denied amount
- The percentage of denied Claims falling under that Denial Category
Selecting a category automatically applies the 'Denial Categories' filter and displays the related Invoice-level details for that specific denial category, as shown in the screenshot below.
Click on the 'View' option next to a category to display the list of Claims denied under that category. You can review, edit, and manage these Claims as needed from the Claims List View.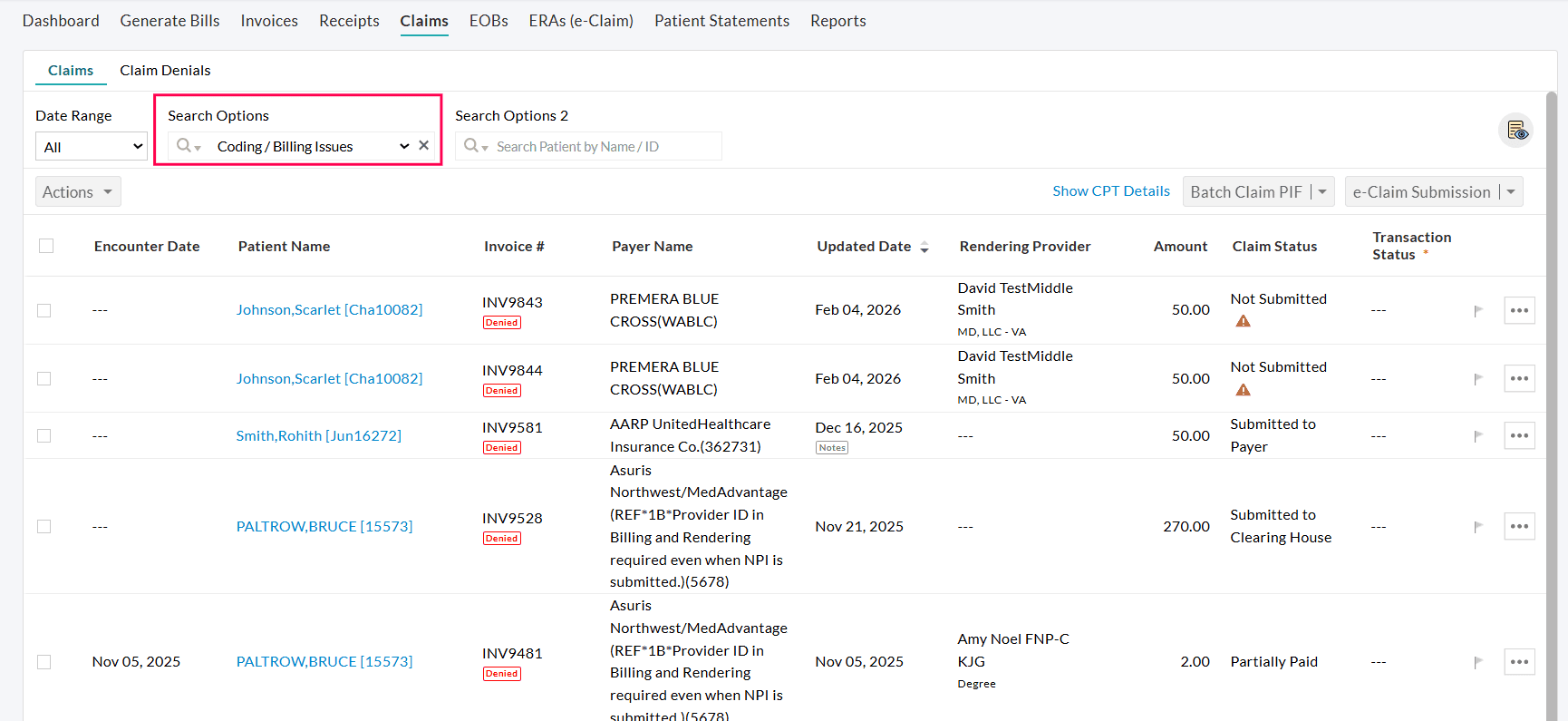
Denied Claims Report
The Denied Claims section displays all denied Claims along with their associated denial details, including:
- Invoice ID and Encounter details
- Denial date and Claim status
- Payer details
- Number of denied CPTs
- CPT-level denial codes and comments
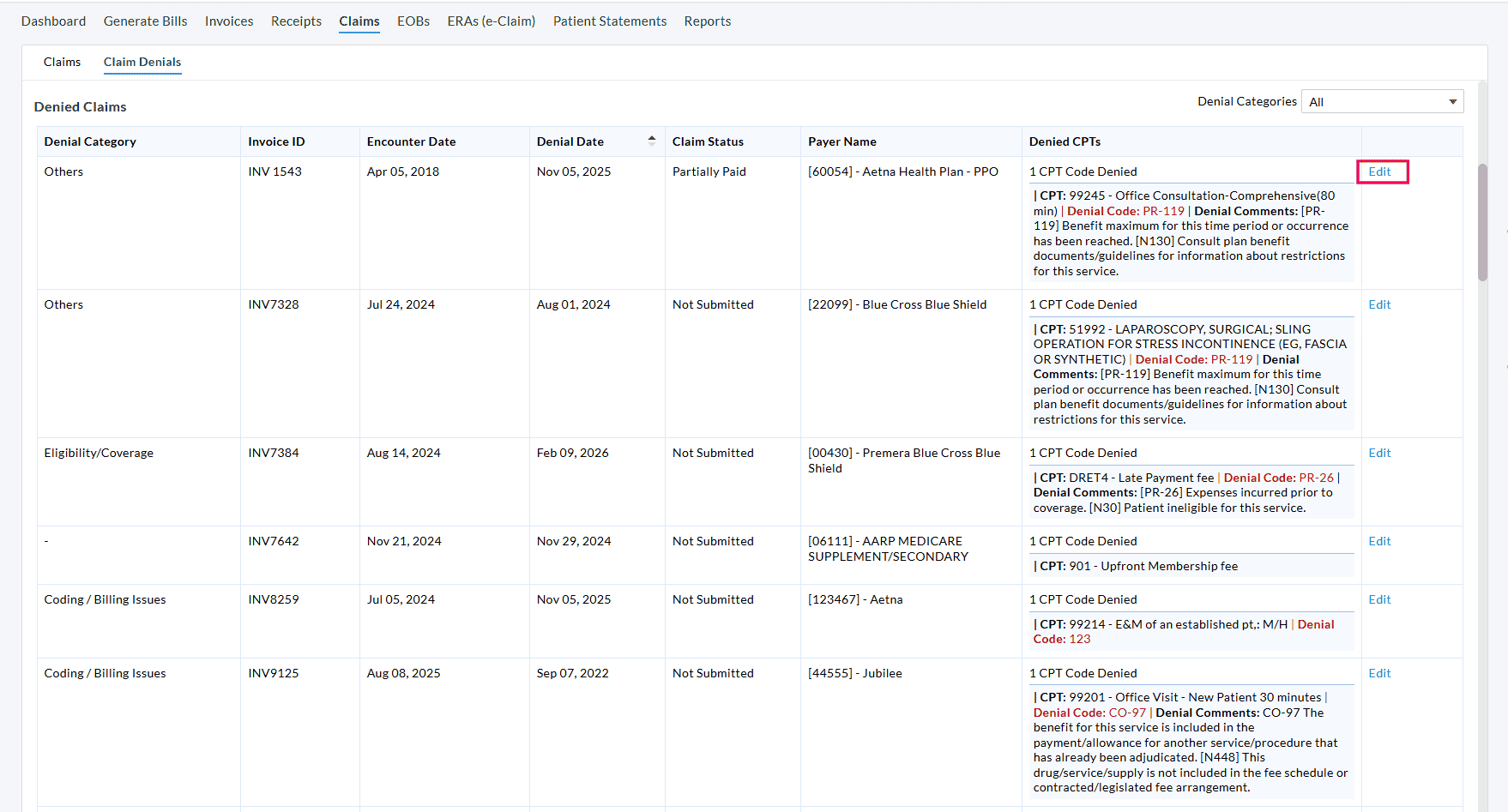
Click 'Edit' to view the Claim and make required corrections or resubmissions.
In the right pane of the Claims view, you can view the denial details of the Claim, including the reason and code for the denial.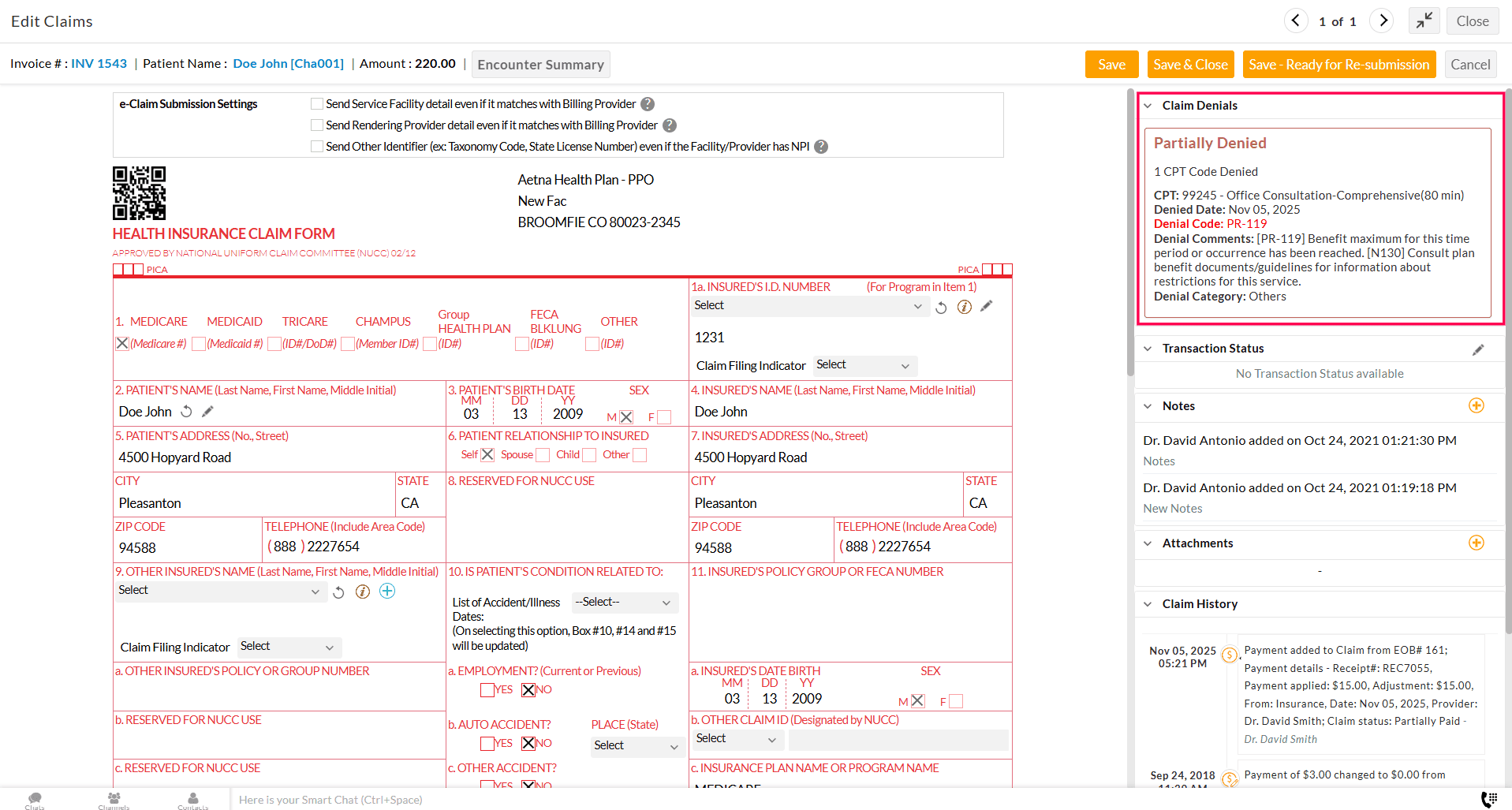
Top 10 Denial Codes
Identify the most frequently occurring denial codes for the selected Facility.
Clicking on the 'View' option displays the Claims grouped by Denial code in the Claims List View.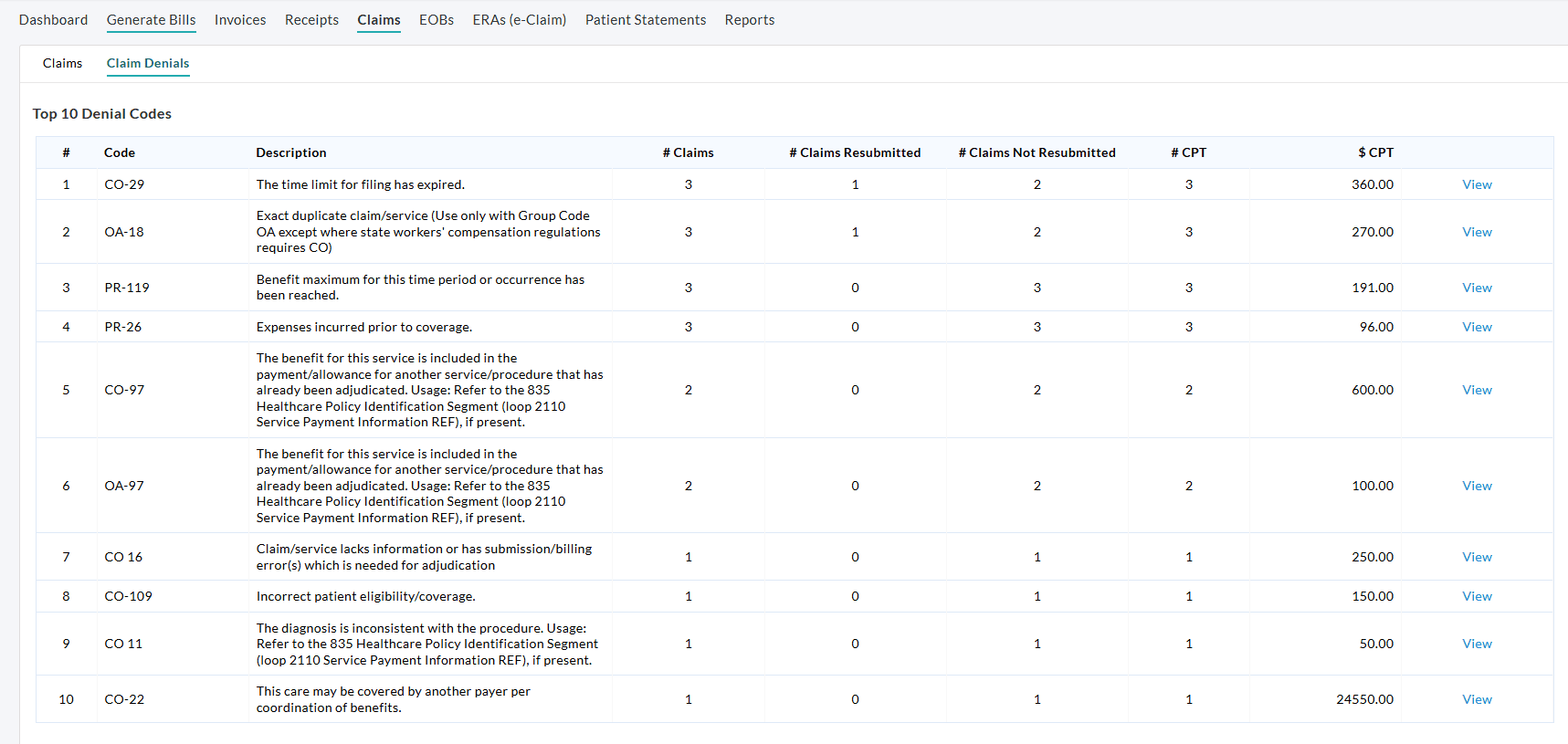
Payer-Wise Denials
This section shows denial details grouped by Payer, enabling Practices to analyze the Payer-specific denial trends.
Click on the 'View' option to list all denied Claims grouped by Payer Code.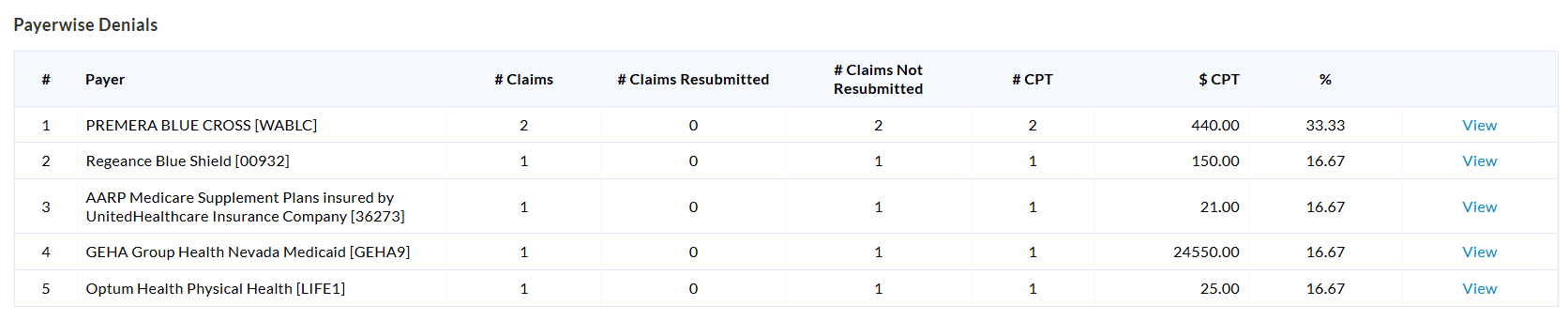
Watchlist - Denied Claims
Denied Claims Watchlist helps the Practice to keep track of all the denied claims that need to be resubmitted and those that are already resubmitted.
- You can access this Watchlist by navigating to 'Billing > Claims' & clicking the Watchlist Icon available in the right corner.
- Denied & Re-submitted Claims
- Denied & not Re-submitted Claims

- Denied & not Resubmitted Claims - It lists the Claims that are denied and not resubmitted.
- Denied & Resubmitted Claims - Claims that are denied and resubmitted to the Payer get listed.
To view the list of Claims in the category, click on the specific watchlist and then click on the respective watchlist count.
Filter - Denied/Rejected Claims
Denied/ Rejected Claims can be listed by selecting the 'Denied/ Rejected Claims' option under the 'Search Options' filter option.

You can also do a finer search using the filter options available, as shown in the screenshot below.
Practices can filter denied Claims based on the Denied Category and Denial Code under 'Billing > Claims > Search Options'.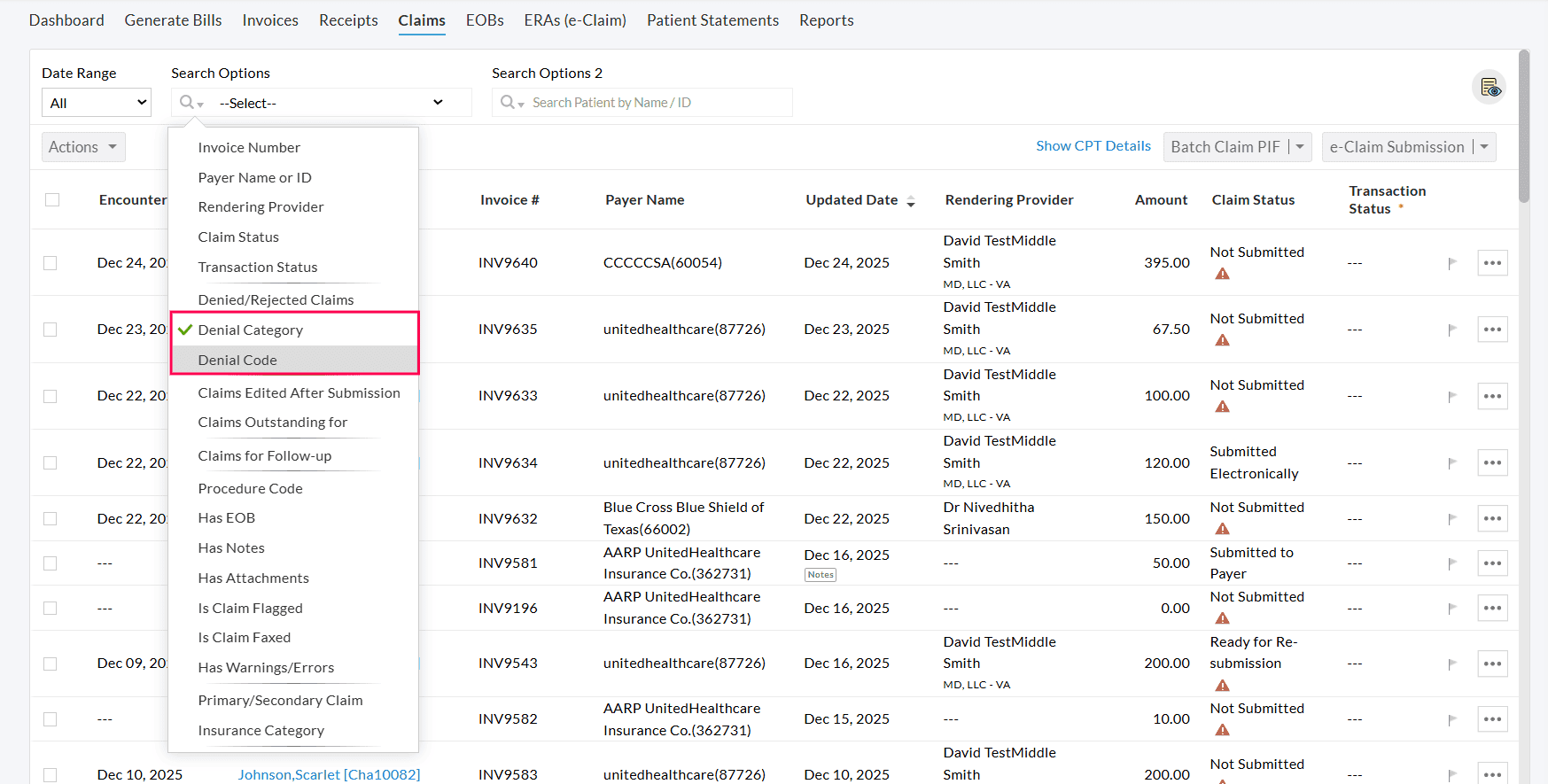
Denial Category
Select the appropriate category to identify Claims denied under that category.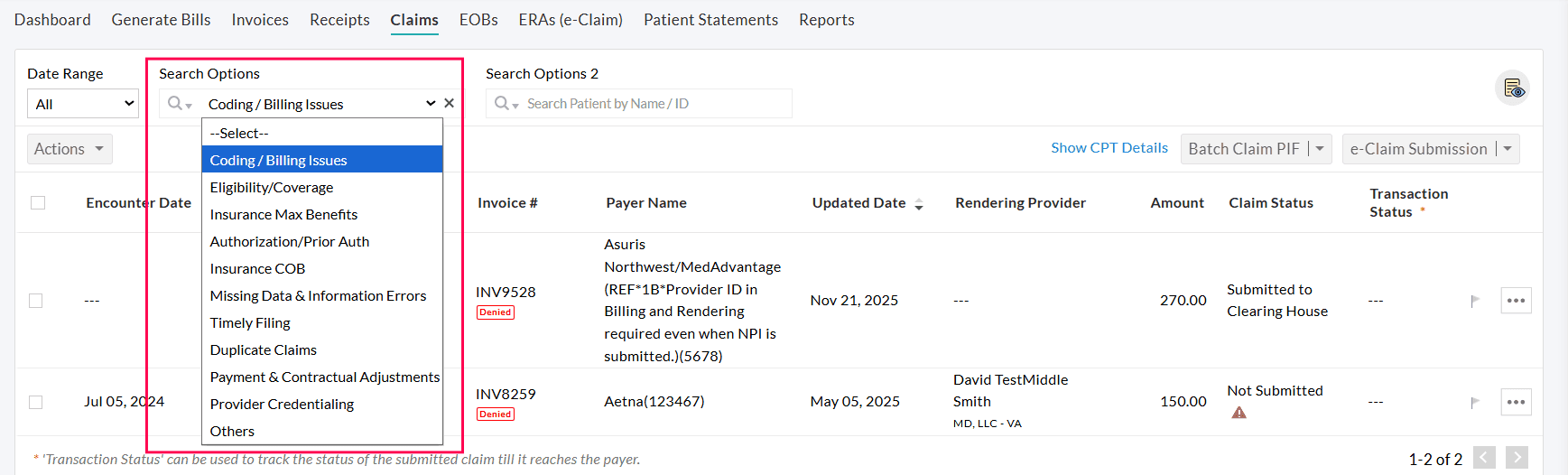
Denial Code
Enter the denial code to filter Claims denied by that specific code.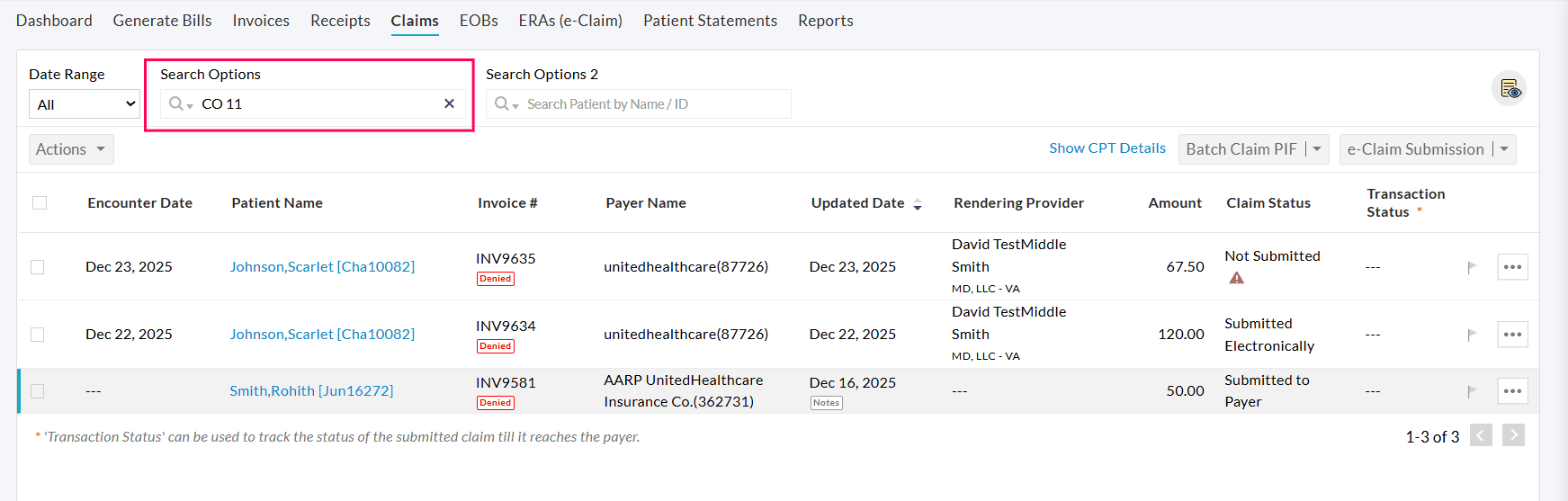
Billing > Reports > Denied Procedures List
Denied Procedure Reports
The Denied Procedure Reports show the list of all the Procedures denied in a particular date range. This report will be shown when 'Item level payments' are enabled for Invoices. Go to the 'Billing > Reports > Denied Procedure Reports' section to generate the reports.
Denied Procedures List
- This report displays all the procedures denied by Payers in the selected date range. It details Invoice information, Denial information, and Payer details of the denied procedures.
- You can group the report by the Patient's name, Package Name, Billing Code for the Procedure Code, Denial Category, Denial Code, Payer ID, Payer Name, Invoice#, Claim Status, Patient Name, Provider, Facility Name, and Facility Code. The report gets listed according to the selected parameter in the 'Group by' option.
- You can also search the Denied Procedures using the Filter options and generate the report.

- Click the 'Show Report' button to view the Denied Procedures Report grouped by the selected parameter.
- You can export the report as a CSV file by clicking the 'Export as CSV' button. Enable the 'Export all the report details with subtotals' option to export all details with subtotals. Else, only the subtotals will get exported.
- To export only the particular columns in the report as a CSV or PDF file, click the 'Settings' icon next to the 'Export Selected Columns' button and drag and drop the column names from the Available Columns to the Selected Columns. Choose the PDF Layout either as a Landscape or a Portrait and click the 'Update' button.
- To save the report as a Custom Report, click the 'Save as Custom Report' button. Enter the Report Name, Description, and choose the Category. To add a new Category, click the 'Add New' link.
Denied Procedures by Code
To list the Denied Procedures grouped by Procedure Codes, follow the steps given below.
- Go to 'Billing > Reports > Denied Procedure Report > Denied Procedures by Code'
- Select the Date Range to list the report. Choose whether to show details by Denial Added Date, Denied Date (As per EOB), Invoice Date, or Encounter Date.

- Click the 'Show Report' button to list the Procedures denied by Procedure Code.
- Click the 'Total Billed Amount' against the line item to view the finer details.
Adding Denials from Secondary Payers
Practices can add denials from the Secondary Payer to the Claims to distinguish denials between Primary and Secondary Payers.

Secondary denials can also be captured in the 'EOBs' section, ensuring all denial-related details are accurately documented.

Handling Claim Rejections and Claim Resubmission
- Rejection of a Claim happens when you send it to the Payer or the Clearinghouse. The rejected Claims are returned to the Practice if there is any missing or invalid information provided in the Claim.
- If your Practice has not signed up for a Clearinghouse, the Payer will send back the rejected Claims through Fax or Paper Mail to the Practice.
- The Claims will be returned with an explanation of rejection from the Payer.
- If a Claim gets rejected by a Clearinghouse, the transaction status will get changed to 'Rejected by Clearinghouse'.
- Click the 'View Transaction History' button to view the transaction details of the Claim.
Claim Resubmission
Once the Claim gets rejected, you need to make changes to the Claim before submitting it to the Payer. You can use the Watchlist or filter option to list all the Rejected Claims.
- Click the 'More Options' (...) icon against the Claim and select the 'Edit Claim (CMS1500)' option.
- Review the Claim and make the necessary changes based on the rejection information.
- On correcting the Claims, click the 'Save-Ready for Re-submission' button to update the Claim.
- The status of the Claim gets changed to 'Ready for Re-Submission' upon updating the changes.
- The corrected Claim gets listed under the 'e-Claim Submission' wizard. Select the Claim and submit it to the Payer electronically.
- If the Practice has not subscribed to E-claims, filter the Claims that are ready for re-submission and download them as PIF files. On editing the Claims, change the status to 'Resubmitted'.
Edit and Preview Claims
To edit the Claim details, follow the steps given below.
- Navigate to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Edit Claim (CMS1500)' option.
- While editing the Claim, the Practices can configure the 'e-Claim Submission Settings' at the Claim level, and this configuration will be used for e-Claim submission.
- Make the required changes to the Claim and click the 'Save' button.
- To edit multiple Claims, select the Claims and click the 'Edit Claims' options under the 'Actions' button.
To preview a Claim, select the 'View Claim' option under the 'More Options' (...) icon against the Claim. You can also select multiple Claims and click the 'Preview Claims' option under the 'Actions' button and preview all Claims one by one.
Any action performed in the Claim gets recorded as Claim History. It includes activities such as Status change, adding notes, adding/updating payment details, adjustment, write-offs, patient responsibility, etc. The Claim history will be shown below the CMS1500 form.
Claims will open in full-screen mode when generated and in Claim preview mode for a better viewing experience.
You can exit full-screen mode anytime for easy navigation. Practices can also show or hide the Claims List in the left pane.


Claim Versioning
Practices can track changes to Claims over a period. Each time a Claim is edited and saved, a new version is automatically generated, providing a detailed history of all modifications.
To view the versions of a Claim, follow the steps below.
- Navigate to the 'Claims' section.
- Select the 'View Claim' option under the 'More Options' (...) icon against the Claim you need to view the versions.


- Click the 'Version#' displayed on the top of the Claim form to view the current Claim version.

- To view the older or previous versions of the Claim, click the drop-down near the recent Version# and select the Claim version to preview.
- Practices can also view the older versions from the 'Claim History' section by clicking the Version# tag.

- The activities of each Claim version are recorded in the 'Claim History' section on the right pane.
- The additional details on E-Claim can be viewed by clicking the 'View More' option against each CPT code.

Resending Corrected Claims and Appeals
- If a Claim gets denied, you may need to resubmit the Claim to the Payer.
- Payers will include an explanation for denial when they send the denied Claim.
- These Claims have to be corrected before sending again to the Payer.
- The corrected Claim tells the Payer that you have sent the Claim to them before, but that you would like it to be re-adjudicated.
Creating a Corrected Claim
The denied Claims need to be corrected and re-submitted to the Payer. To create a corrected Claim, follow the steps given below.
- Go to 'Billing > Claims'
- Select the Claim denied by the Payer.
- Click the 'More Options' (...) icon against the Claim and select the 'Edit Claim (CMS1500)' option.
- Review the Claim and adjust the incorrect information according to the explanation of denial sent by the Payer.
- Select the Resubmission Code as '(07) Replacement' in Box#22 of the CMS1500 Claim form.
- Enter the 'Original Reference No' in Box#22. Entering the reference# differs the corrected Claim from the Original Claim, thus eliminating sending duplicate Claims.

- Click the 'Save-Ready for Re-submission' button to update the Claim and to change the Claim status to 'Ready for Re-Submission'. The corrected Claim will get listed under the 'e-Claim Submission' wizard. Select the Claim and submit it to the Payer.
- For the Claims received through Fax or Paper Mail, resubmit the Claim and change the Claim Status to 'Resubmitted'.
Appeals
- If the Payer disagrees with any item or service provided and withholds reimbursement payment, the Practice can appeal those Claims to be re-processed.
- You need to gather the following information.
- Appeal Letter: It is a cover letter or summary that explains to the Payer why you’re appealing the Claim and how your documentation supports those reasons.
- Supporting documentation: This includes progress notes, Patient labs, or other formal documentation that support your Claim.
- Claim Reference#: At times, an appeal gets lost or processed as a duplicate because the Payer cannot connect the appeal to the original Claim.
- Follow the specific insurance appeals process: Make sure you look into the insurance company's appeals process before submitting an appeal.
- On collecting the required information, the appeal letter can be sent through Fax or Paper Mail.
Claim Follow-up
Claim Follow-up is important as it prevents gaps in the Billing cycle and keeps revenue flowing smoothly.
To set Claims for follow-up, go through the steps given below.
- Navigate to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Set Claim Follow-up' option

- Choose the period within which the Claim needs a follow-up.
- Click the 'Add' button to set the follow-up for the Claim.
To view the Claims marked for follow-up, follow the steps given below.
- Select the 'Claims for Follow-up' option under the 'Search Options'.
- Choose the 'Claims for Follow-up' option to list the Claims marked for follow-up.
- You can choose the appropriate option from the drop-down list, as shown in the screenshot.

To clear Claim follow-up, follow the steps given below.
- Select the 'Claims for Follow-up' option under the 'More Options' (...) icon against the Claim.
- Select the 'Claim is followed up' checkbox option.
- To view the Claims that are followed up, select the 'Claims followed up' option from the 'Claims for follow-up' search option.
Usage of 'Date Range'
This filter lists the Claims based on the selected Date Range. By default, all Claims of the chosen Facility get listed. You can select one of the pre-configured filters, as shown in the screenshot below, or enter your custom date range for the filter.

Claim Search Options
The Claims get listed based on the search options available, as shown in the screenshot below.
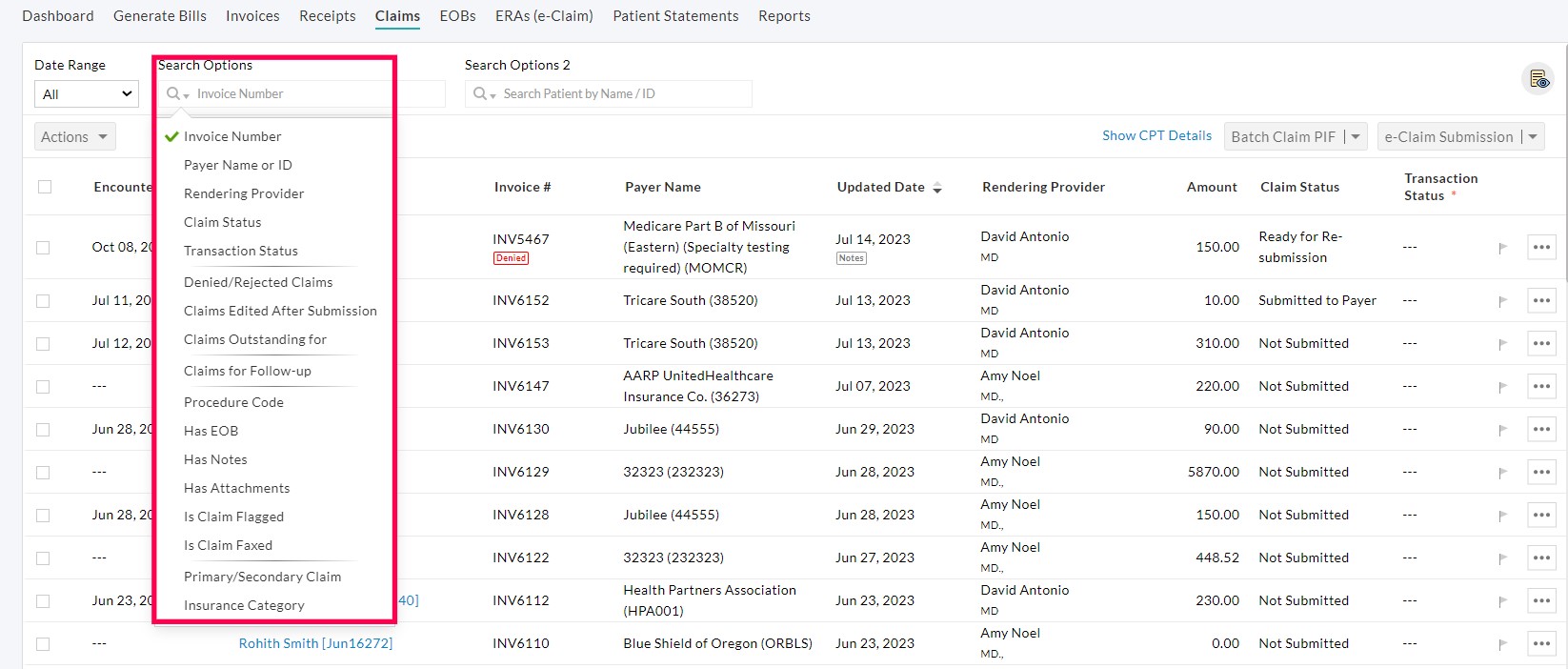
- Invoice Number: Search the Claims by entering the Invoice Number for which the Claims are generated.
- Payer Name or ID: Enter the Payer Name or ID to list the Claims generated for a particular Payer.
- Rendering Provider: List the Claims based on their 'Rendering Provider'.
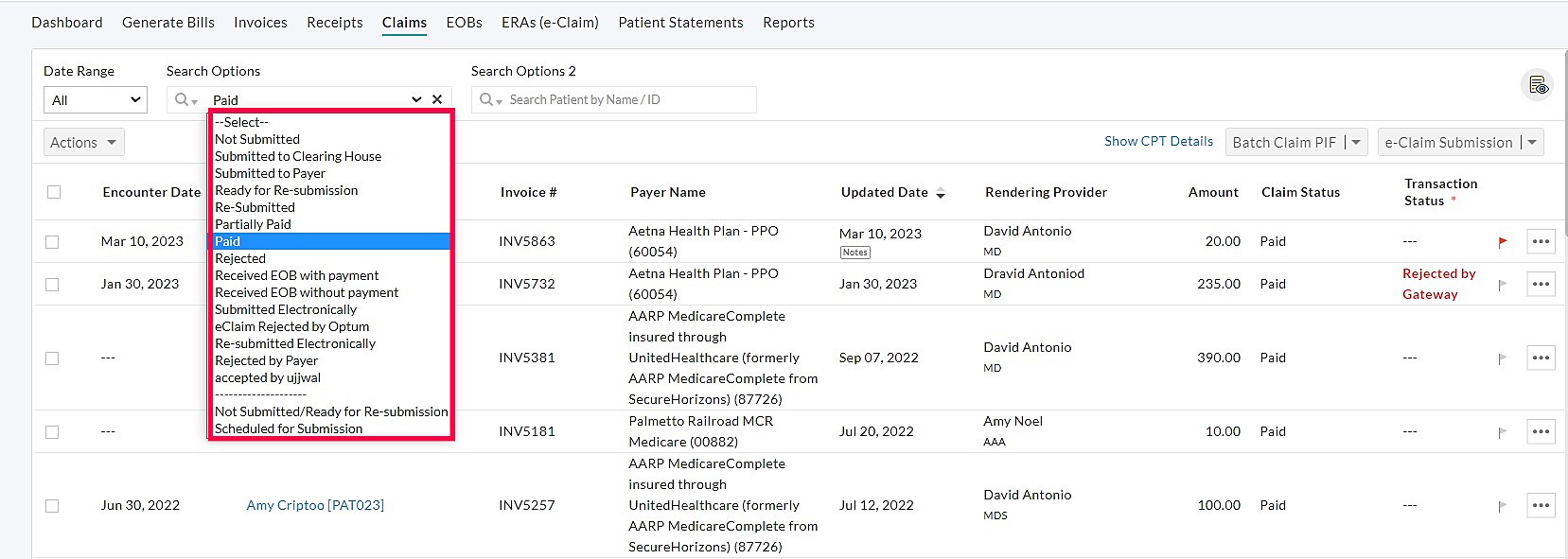
- Claim Status: Search the Claims based on their Status Viz. Submitted, Submitted to Clearing House, Submitted to Payer, etc.
- Transaction Status: Search the Claims based on their Transaction Status.
- Denied/Rejected Claims: Lists all the Denied/Rejected Claims. Choose the required options from the drop-down menu.
- Denied & Not-Resubmitted Claims: Claims that are denied and not re-submitted to the Payer get listed.
- Denied & Re-submitted Claims: Claims that are denied and re-submitted to the Payer get listed.
- All Denied Claims: Lists all the Denied/Rejected Claims in a selected period.
- Claims edited after Submission: All Claims that are edited after submission to the Payer get listed.
- Claims Outstanding For: Lists the Claims that are outstanding after N number of days viz. 10 days, 20 days, 30 days, etc. Select the range from the drop-down menu.
- Claims for Follow-up: This option lists the Claims added for follow-up, upcoming Claims for follow-up, and Claims followed up. You can also choose to list the Claims for follow-up added by you.
- Procedure Code: List all the Claims with a specific Procedure Code.
- Has EOB: You can filter the Claims with no EOB, with one EOB, and with more than one EOB.
- Has Notes: Claims with or without Notes get listed.
- Has Attachments: Claims with or without Attachments get listed.
- Is Claim Flagged: Select this option to list the Flagged or Un-flagged Claims.
- Is Claim Faxed: Select this option to list the Claims that are faxed or not- faxed.
- Primary/Secondary Claim: Choose this option to list only the Primary Claim or Secondary Claims. You can also select the option from the drop-down to list accordingly.
- Claims with Patient Secondary Payer & No Secondary Claim: You can choose this filter to generate Secondary Claims for the Patients with Secondary Payer.
- Claims having PR with Patient Secondary Payer & No Secondary Claim: Choose this option to filter the Claims having PR with Patient Secondary Payer and no Secondary Claim. You can generate Secondary Claims for the Claims with Patient Responsibility.

- Insurance Category: Lists the Claims based on the Insurance category viz. Primary, Secondary, Tertiary, Auto (PIP/MVA), Workers' Compensation, & Others.
Additional Search Option
Practices can now filter claims efficiently using two search options available in the Claims section.
For instance, if the Practices need to follow up on the Claims of a specific Payer, they can use the filters with a combination of 'Claims for Follow-up' & 'Payer Name or ID' as shown below.

Claim Actions and Bulk Actions

Add Notes
Notes can be added to a Claim by following the steps given below.
- Go to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Add/ View Notes' option.
- Enter the details and click the 'Add' button.
- Notes added earlier will get listed under the 'Past Notes' section.

To add Notes to multiple Claims, follow the steps given below.
- Select the Claims for which notes to be added.
- Click the 'Actions' button and select the 'Add Notes' option.
- Enter the details and click the 'Add Notes' button.
- To list the Claims with Notes, select the 'Has Notes' option under the 'Search Options' drop-down.
- Claims with Notes are labeled with the 'Notes' tag below the Updated Date.
Flag Claim
The Practice can flag the important Claims that need further analysis/work. The Claims can be flagged/un-flagged by following the steps given below.
- Go to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Flag Claim' option.
- The Claim gets flagged and can be un-flagged by clicking the Flag icon again.
- To flag multiple Claims in a single click, select the Claims to be flagged.
- Click the 'Actions' button and select the 'Flag Claims' option.
- To un-flag the multiple Claims, select the flagged Claims and click the 'Clear Flags' option under the 'Actions' button.
- To list the flagged/un-flagged Claims, select the 'Is Claim Flagged' option under the 'Search Options' drop-down.
Change Status
To change the Claim status, follow the steps given below.
- Go to 'Billing > Claims'
- Click the 'More Options' (...) icon against the Claim and select the 'Change Status' option.

- Select the Status to be changed and click the 'Update Button'.
To change the status of multiple Claims, follow the steps given below.
- Select the Claims for which the status needs to be changed.
- Click the 'Actions' button and select the 'Change Status' option.
- Select the status and click the 'Update' button.
Add Attachment
Practices can add attachments to a Claim from the Local Drive or Charm Documents. To attach a document to a Claim, follow the steps given below.
- Go to 'Billing > Claims' and click the 'More Options' (...) icon against the Claim.
- Select the 'Add/View Attachments' option.

- From Local Drive
- Click the 'Choose File' button.
- Browse and add the file from your system.
- Select the 'Attachment Type' from the drop-down menu.
- To add more attachments, click the 'Add More' option.
- Click the 'Attach' button to add the attachment(s) to the Claim.

- From Charm Documents
- Select 'Charm Documents'. All the Practice and Patient documents get listed.
- Choose one or more files to be attached to the Claim and select the appropriate Attachment Type.
- Click the 'Attach' button.
Note: The Practice documents can be added under the 'Settings > Documents' section, and the Patient documents can be added under the 'Patient Dashboard > Documents' section.


- To search the Claims with attachments, select the 'Has Attachments' option under the 'Search Options' drop-down.
- Claims with attachments are labeled with the 'Pin' icon.
Handling Secondary Claims
This document outlines when to generate a Secondary Claim and the steps to generate the Secondary Claim.
When to generate a Secondary Claim
To generate a Secondary Claim, the following conditions should be satisfied.
- Patients should have active Secondary Insurance.
- Primary Claim payments should have Patient Responsibility (PR), or some procedures were not covered/paid by the Primary Payer.
Generating Secondary Claims
- Use the claim filter 'Primary/Secondary > Claims have PR with Patient Secondary Payer & No Secondary Claim' to see all the claims available for secondary insurance processing.

- Choose a Primary Claim, click on the 'Generate Secondary Claim (CMS1500)' option under the 'More options' (...) icon against the Primary Claim. If the Primary Claim is in 'Not Submitted' status, the Secondary Claim cannot be generated.

- Clicking on the 'Generate Secondary Claim' option opens up the Claim wizard. This pre-populates all the Claim information from the Primary Claim except the following such as, the Prior Authorization Number of the Primary Claim, Original Reference Number used if the Primary Claim is resubmitted, Secondary Insurance for the Patient is chosen as Primary Insurance for this Secondary Claim; Primary Insurance in the Primary Claim is chosen as Secondary Insurance in the Secondary Claim.
- Payment received from the Primary Payer should be entered in the 'Amount Paid (Copay)(29)' field.
- Go through the CMS1500 form claim wizard, verify the details, and save the claim.
When Practice is submitting Claims using Print Image File(PIF)
- Print the secondary Claim on CMS 1500 form.
- Print the Explanation of Benefits (EOB) document received from the Primary Payer.
- Send the Claim CMS form along with the Primary EOB to the Secondary Payer either by fax or by mail.
When Claims are submitted electronically (e-Claims package enabled Practices)
When electronic Claim submission is enabled for the Practice, the Secondary Claim with the Primary EOB information can be sent electronically to the Secondary Payer.
The Primary EOB information should be entered in the 'Adjudication Details' section, shown at the bottom of the CMS1500 Form claim wizard. The following sections explain the procedure for adding EOB details in the Claim wizard.
When EOB information is entered manually or pulled electronically (a feature in the e-Claims package), the adjudication details will be filled in automatically.

Examples
Refer to the sample EOB shown below. It has two CPTs with a payment of $4.30 for CPT 87880 and $113.06 for CPT 99214, along with adjustments and PR.

- Clicking on the 'Add EOB' option opens the 'EOB Detail View' dialog with all Claim CPTs populated by default.
- For CPT 87880, the payment is $25.05. It is entered in the 'Paid Amount' field.
- This CPT has an adjustment of $0.95, which is to be added using the 'Add Adjustment' option with the 'CO-Contractual Obligation' Group.
- Similarly, another CPT 99214 has a payment of $113.06. It gets entered in the 'Paid Amount' field. It also has a Patient responsibility of $20 and a Contractual Obligation of $28.94. It gets entered in a separate adjustment with the Group as 'PR-Patient Responsibility' and 'CO-Contractual Obligation' respectively.
- Update the EOB details.

The EOB information added will be shown in a line item.
Note: Secondary Claims not listed in the Claim report available under the 'Billing > Reports' section.
Handling Billing when provider leaves the Practice
To figure out how much the Provider should be paid when they leave the Practice, it is essential to work out what they are owed. The following reports under the 'Billing > Reports' section help the Practice to have a clear view of how much the Provider should be paid. These reports will be available only if the item-level payments are enabled for the practice.
Payment Collection for Procedures by Provider
- This report lists under the 'Provider Reports (Based on Provider selected in Invoice)' section.

- This report shows the payment collection of Procedures in total grouped by Provider.
- Choose the Invoice payment date range and generate the report.
- Total payment collected for Procedures by each Provider in the Practice gets listed.
- Click the 'Total Payment' link against the Provider to view the finer details.
Payment Collection for Products by Provider
- This report lists under the 'Provider Reports (Based on Provider selected in Invoice)' section.

- This report shows the payment collection of Products in total grouped by Provider.
- Choose the Invoice payment date range and generate the report.
- Total payment collected for Products by each Provider in the Practice gets listed.
- Click the 'Total Payment' link against the Provider to view the finer details.
Payment Collection for Procedures
- This report lists under the 'Collection Reports' section.
- This report shows the payment collected for Procedures in any selected date range.

- The report runs based on the date on which the payment is applied to Procedure/Invoice.
- Practices can use this report to calculate Provider commission based on the Procedure collection.
- Choose the date range and group the report by 'Provider'.
- Total payment collected for Procedures by each Provider in the Practice gets listed.
- Click the 'Total Payment' link against the Provider to view the finer details.
Payment Collection for Products
- This report lists under the 'Collection Reports' section.
- This report shows the payment collected for Products in any selected date range.

- The report runs based on the date on which the payment is applied to Procedure/Invoice.
- Practices can use this report to calculate Provider commission based on the Product collection.
- Choose the date range and group the report by 'Provider'.
- Total payment collected for Products by each Provider in the Practice gets listed.
- Click the 'Total Payment' link against the Provider to view the finer details.
Procedures by Provider
- This report lists under the 'Procedure Reports' section.
- This report shows the total payment charged for the Procedures by each Provider in the selected date range.
- Click the 'Total Charge after Discount and Tax' link against the Provider to view the finer details.

Default ID Qualifier for Billing
Practices can set default ID Qualifier for Rendering Provider which will be chosen automatically in Claim generation.
When the Providers have more than one ID Qualifier, setting up a default ID Qualifier will save time in Claim generation.
To set a default ID Qualifier for Practice Member, follow the steps given below.
- Go to 'Settings > Facility > Facility Members'
- Click on the 'More Options' (...) icon against the Practice Member you want to set the default ID Qualifier and select the 'Edit' option.
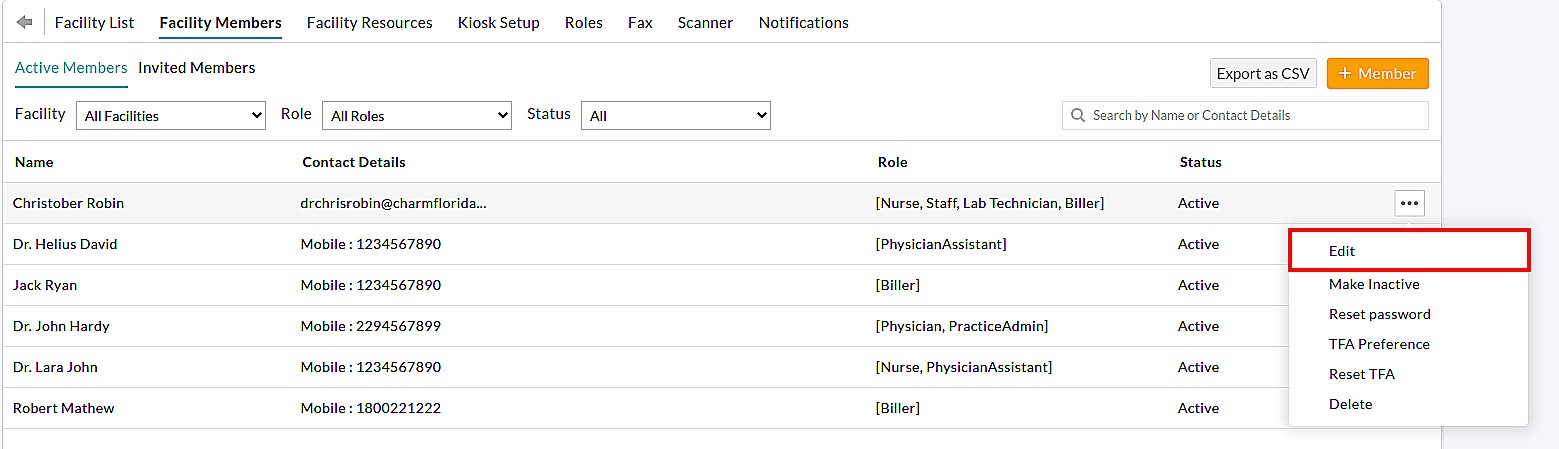
- Click on the 'Use in Billing Default' option available against each ID Qualifier.
- Once set, this ID Qualifier will be chosen automatically for the Provider in the Claim generation.

Claims - Watchlist
A Watchlist helps the Practices to get an overview of important Claim information all in one place. Members of the Practice can click on individual items to get more specific details and take further action as needed.

- Not Submitted Claims: Claims that are not submitted to the Payers get listed.
- Rejected Claims: Claims that are rejected by the Payer or Clearinghouse get listed in this section.
- Denied & not Re-submitted Claims: Claims that are denied by the Payer and are not re-submitted get listed in this section. The Practice can resubmit these Claims to the Payer.
- Denied & Re-submitted Claims: Claims that are denied and resubmitted to the Payer will appear here.
- Claims for Follow-up: Claims that are marked for follow-up get listed.
- ERAs- Unmapped EOBs: List the number of EOBs with no mapping Claims in the ERAs section.
- ERAs- Payment Failures: List the number of EOBs with payment failures in the ERAs section.
Claims - Reports
The Claim Report gives you a detailed overview of all Claims created in a given period. You can customize it to show a particular range of Claims with the filters. Go to the 'Billing > Report' section to view the following reports.
Claims List
- This report lists the Claims generated in the selected Date Range.
- You can group the report by Facility Name, Patient Name, Invoice#, Payer Name, Payer ID, Insurance Category, Prior Authorization Number, Billing Provider, Tax ID, Referring Provider, and Facility Code.
- The report gets listed according to the selected parameter in the 'Group by' option.
- You can also search the Invoices using the Filter options and generate the report.
- Choose the Status of the Claims to be listed.

- Click the 'Show Report' button to view the Claim Report grouped by the selected parameter.
- You can export the report as a CSV file by clicking the 'Export as CSV' button. Enable the 'Export all the report details with subtotals' option to export all details with subtotals. Else, only the subtotals will get exported.
- To export only the particular columns in the report as a CSV or PDF file. Click the 'Settings' icon next to the 'Export Selected Columns' button and drag and drop the column names from the Available Columns to the Selected Columns. Choose the PDF Layout either as a Landscape or a Portrait and click the 'Update' button.
- To save the report as a Custom Report, click the 'Save as Custom Report' button. Enter the Report Name, Description, and choose the Category. To add a new Category, click the 'Add New' link.
Claims Aging Report by Payer
- This report shows the outstanding amount that the Practice needs to collect from the Payers.
- This outstanding amount is grouped based on the age of Claims. This report does not consider Invoices or Claims of visits that are paid fully.
- To view all the Invoices of the payer, click on the 'Total' link and unselect the 'Show only Invoices with due' option.

Claims by Patient
- Go to 'Billing > Reports > Claim Reports > Claims by Patient'
- This report lists the Claims grouped by Patient name.
- Choose to show the Claims whether by Claim Date or Encounter Date and select the Date Range.
- Click the 'Show Report' button to generate the report.

- Download the information in CSV format with a single click on the 'Export as CSV' button.
Claims by Provider
- This report lists the Claims grouped by Provider.
- Choose to show the Claims either by Claim Date or Encounter Date and select the Date Range.
- Click the 'Show Report' button to generate the report.

Claim Procedures List
- This report shows the list of 'Procedure Codes/Services' that are billed to the Payer/Insurance Company.
- All the details shown in Box # 24.A to 24.J in 'CMS1500 Form' of Claim will be shown in this report.
- This report can also be filtered based on the Place of Service, Modifiers, Dx Codes, etc.

- To get the CSV file, click the 'Export as CSV' button.